Updated on: July 29, 2025
A dilated aortic root is often an incidental finding on echocardiogram or CT but can be a harbinger of serious aortic pathology. Left unmonitored or poorly documented, it can progress to aneurysm formation, dissection, or even sudden cardiac death. For clinicians, especially cardiologists and internists, clear and accurate documentation of this condition is critical—not just for patient safety, but also for effective coding, billing, and longitudinal care planning.
In this guide, we’ll explore:
-
What a dilated aortic root means and why it matters
-
Associated conditions and differential diagnosis
-
Proper ICD-10 coding, including I77.810 – Aortic ectasia
-
Documentation challenges and examples
-
How DocScrib helps automate and enhance cardiovascular note-taking
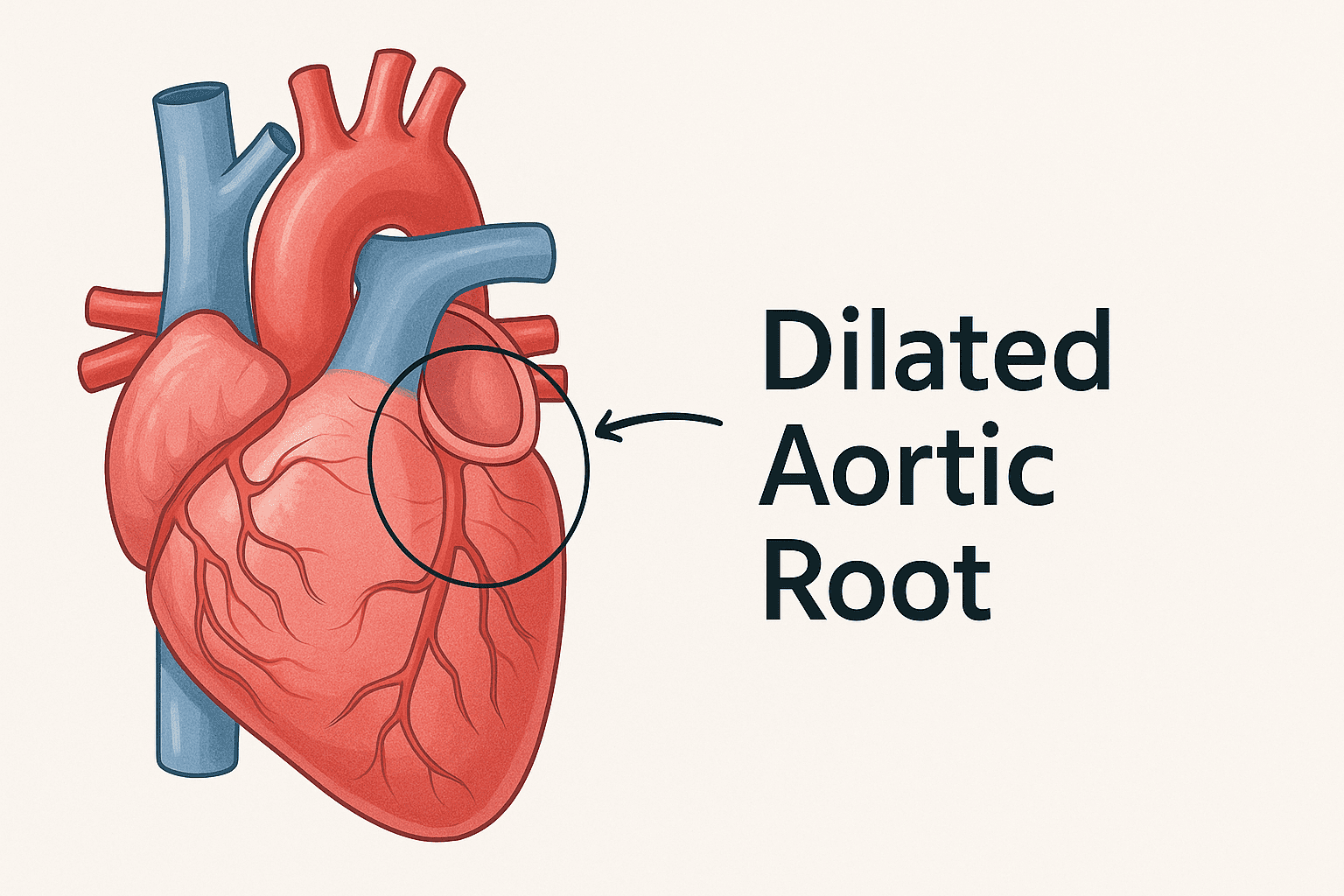
What is a Dilated Aortic Root?
The aortic root is the section of the aorta attached to the heart, where the aortic valve and coronary arteries originate. A dilation of the aortic root means that this segment is wider than normal—commonly considered dilated if:
-
≥4.0 cm in diameter in adults, or
-
Z-score ≥2 in pediatric populations
Clinical Significance
Aortic root dilation can indicate early aortic aneurysm, aortopathy, or connective tissue disorders like Marfan syndrome or Loeys-Dietz syndrome. It often requires regular imaging follow-up, medication management, and in some cases, surgical intervention.
Causes of Dilated Aortic Root
Common Etiologies
| Category | Example Conditions |
|---|---|
| Genetic syndromes | Marfan, Ehlers-Danlos, Loeys-Dietz |
| Hypertension | Long-standing systemic pressure load |
| Bicuspid aortic valve | Congenital structural abnormality |
| Inflammatory diseases | Takayasu arteritis, syphilitic aortitis |
| Aging & degeneration | Aortic medial degeneration (cystic) |
| Trauma or iatrogenic | Post-surgical, post-intervention changes |
Symptoms (Often Absent Until Complications)
-
Asymptomatic in early stages
-
Chest pain or discomfort
-
Shortness of breath
-
Murmur (from aortic regurgitation)
-
Rare: signs of dissection or rupture
ICD-10 Coding for Dilated Aortic Root
Primary Code
I77.810 – Aortic Ectasia
-
Appropriate when the aortic root is dilated but does not yet meet criteria for aneurysm
-
Used in echocardiogram findings or incidental CT reads
-
Describes localized, mild to moderate dilation
Related Codes
| ICD-10 Code | Description |
|---|---|
| I71.1 | Thoracic aortic aneurysm, ruptured |
| I71.2 | Thoracic aortic aneurysm, nonruptured |
| I35.1 | Aortic valve insufficiency (if regurgitation present) |
| Q87.4 | Marfan syndrome |
| Z13.6 | Encounter for genetic screening (for inherited aortopathy) |
📌 Use I77.810 when the dilation is clearly documented but not classified as aneurysmal. If the dilation meets aneurysm criteria (>4.5–5.0 cm), consider I71.x codes instead.
Sample Documentation for Aortic Root Dilation
Echocardiogram Report:
“Aortic root diameter is 4.2 cm. Normal aortic valve function. No dissection or aneurysm noted.”
SOAP Note Example:
Subjective:
Patient denies chest pain, palpitations, or dyspnea. No family history of aortic aneurysms.
Objective:
BP: 132/78 mmHg. HR: 72 bpm. Normal S1/S2. Diastolic murmur absent.
Assessment:
Mild dilation of aortic root (4.2 cm) noted on recent echocardiogram. No signs of aneurysm or dissection. No symptoms currently.
Plan:
-
Monitor with repeat echo in 12 months
-
Maintain BP <130/80
-
Genetic screening due to tall stature and positive family history
-
ICD-10 Code: I77.810 – Aortic ectasia
Clinical Management: When to Refer and Intervene
| Aortic Root Diameter | Action |
|---|---|
| 3.0–3.9 cm | Normal range, no action |
| 4.0–4.4 cm | Mild dilation; monitor annually |
| 4.5–4.9 cm | Borderline aneurysmal; consider CTA/MRI |
| ≥5.0 cm | Aneurysmal; refer to cardiovascular surgery |
Referral Indications
-
Growth rate >0.5 cm/year
-
Presence of aortic regurgitation
-
Symptoms (e.g., chest pain, syncope)
-
Associated syndromes like Marfan, Loeys-Dietz
Importance of Accurate Documentation
Aortic ectasia can often be underdocumented due to its incidental nature. Yet proper coding and follow-up are essential for:
-
Surveillance imaging scheduling
-
Aneurysm progression tracking
-
Reimbursement and risk adjustment
-
Flagging for genetic or surgical referrals
Documentation Pitfalls to Avoid
🚫 Vague terms like “borderline dilation” without exact measurement
🚫 Missing association with symptoms or physical findings
🚫 No longitudinal tracking plan
🚫 Inaccurate coding as aneurysm when dilation is <4.5 cm
How DocScrib Simplifies Cardiovascular Documentation
AI-powered tools like DocScrib make it easier for cardiologists and internists to capture subtle imaging findings, track disease progression, and auto-suggest relevant ICD-10 codes—like I77.810—within seconds.
With DocScrib, You Can:
✅ Dictate echocardiogram findings, and get a structured note instantly
✅ Autogenerate ICD-10 codes based on symptom and imaging mentions
✅ Flag findings like mild aortic ectasia for follow-up reminders
✅ Reduce time spent charting by over 70%
✅ Seamlessly integrate with your EHR or cloud platform
Experience AI-powered documentation for cardiology today
👉 Book your personalized demo now
Quick Reference Table: Aortic Root Dilation Coding
| Clinical Scenario | ICD-10 Code(s) |
|---|---|
| Mild dilation (3.9–4.4 cm) | I77.810 |
| Thoracic aortic aneurysm (>5.0 cm) | I71.2 or I71.1 |
| Aortic regurgitation due to root dilation | I35.1 + I77.810 |
| Aortopathy with Marfan syndrome | Q87.4 + I77.810 |
| Pre-surgical or surgical follow-up case | Z09 + I77.810 |
FAQs About Dilated Aortic Root
Q1: Is a dilated aortic root dangerous?
Not always. Mild dilation is often benign, but progression to aneurysm can pose significant risk if not monitored.
Q2: Can a dilated aortic root return to normal size?
Rarely. While medications like beta-blockers can slow progression, reversal is uncommon.
Q3: Should I always code I77.810 when root dilation is seen?
Yes, if documented clearly in the imaging report—even if incidental. This helps track progression over time.
Q4: How does DocScrib detect such incidental findings?
DocScrib captures dictated or typed clinical notes and imaging impressions, then flags relevant codes like I77.810 for clinician review.
Q5: Is follow-up imaging required?
For measurements >4.0 cm, annual echo or CTA is typically recommended, unless faster growth or syndromic features are present.
Conclusion
Dilated aortic root may seem like a minor radiological finding, but it carries long-term cardiovascular risks that require vigilant monitoring, accurate ICD-10 coding, and clear documentation. Using the correct code—I77.810 – Aortic ectasia—ensures clinicians can track progression and intervene appropriately.
Tools like DocScrib are revolutionizing cardiology documentation by making charting faster, smarter, and more accurate.
👉 Try DocScrib for your cardiology team – book your free demo now