Updated on: July 20, 2025
Accurate coding for Major Depressive Disorder (MDD) using ICD-10 is critical for effective treatment, proper billing, and maintaining reliable health data. This guide breaks down the most-used codes, their classifications, and how to document MDD correctly while avoiding common mistakes. Here’s what you need to know:
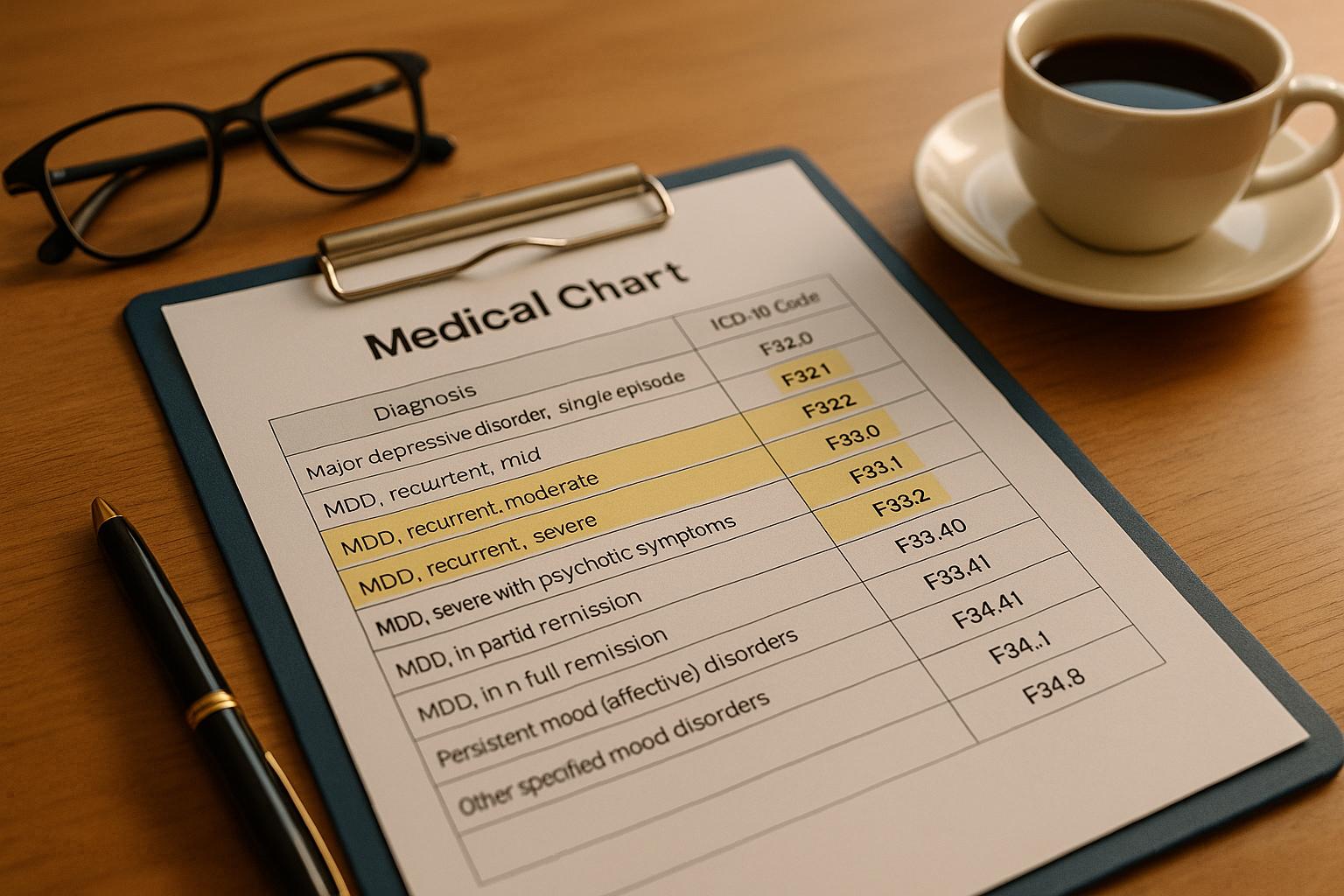
- ICD-10 Codes for MDD:
- Single depressive episodes use F32.x codes, ranging from mild (F32.0) to severe with psychotic features (F32.3).
- Recurrent episodes are coded as F33.x, such as F33.1 for moderate recurrent depression.
- Related conditions like dysthymia (F34.1) and postpartum depression (F53.0) have separate codes.
- Why It Matters: Accurate coding affects insurance claims, treatment planning, and compliance with healthcare standards. Errors can lead to claim denials and skewed health statistics.
- Documentation Tips:
- Include symptom severity, duration, and their impact on daily life.
- Use tools like PHQ-9 to assess symptoms and ensure detailed, timely notes.
- Avoid vague terms like “history of” for active symptoms.
- Best Practices: Regularly update codes, conduct chart audits, and use structured formats like SOAP notes. Leverage technology, such as AI-powered tools, to streamline documentation and maintain compliance.
Proper documentation not only supports patient care but also ensures financial and regulatory accuracy. Keep these guidelines in mind to improve your MDD coding and documentation process.
Sequencing of Codes: Depression and Suicide Ideation Codes
ICD-10 Codes for MDD
Using precise ICD-10 codes for Major Depressive Disorder (MDD) is essential for accurate diagnoses, effective treatment planning, and proper billing. These codes fall into two main categories: F32 codes for single depressive episodes and F33 codes for recurrent episodes, covering a range from F32.0 to F33.9.
F32 Codes: Single Episode of Major Depressive Disorder
F32 codes are used to document a patient’s first depressive episode. If additional episodes occur, F33 codes are applied. These codes classify the severity of the episode, the presence of psychotic features, and the remission status. The severity is determined by factors like mood changes, reduced energy levels, and a noticeable decrease in activity.
| ICD-10 Code | Description |
|---|---|
| F32.0 | Major depressive disorder, single episode, mild |
| F32.1 | Major depressive disorder, single episode, moderate |
| F32.2 | Major depressive disorder, single episode, severe without psychotic features |
| F32.3 | Major depressive disorder, single episode, severe with psychotic features |
| F32.4 | Major depressive disorder, single episode, in partial remission |
| F32.5 | Major depressive disorder, single episode, in full remission |
| F32.9 | Major depressive disorder, single episode, unspecified |
For instance, F32.0 (Mild) applies when symptoms are present but the individual can still manage most daily tasks. On the other hand, F32.2 (Severe without psychotic features) indicates a significant loss of functionality, while F32.3 (Severe with psychotic features) includes symptoms such as hallucinations or delusions. Codes like F32.4 and F32.5 track recovery progress, and F32.9 is used when specific details about the episode are unavailable.
For cases involving repeated depressive episodes, the F33 codes should be referenced.
F33 Codes: Recurrent Episode of Major Depressive Disorder
F33 codes document recurrent depressive episodes in individuals with no history of manic episodes . This category highlights the chronic nature of MDD and aids in planning long-term treatment strategies.
| ICD-10 Code | Description |
|---|---|
| F33.0 | Major depressive disorder, recurrent, mild |
| F33.1 | Major depressive disorder, recurrent, moderate |
| F33.2 | Major depressive disorder, recurrent, severe without psychotic features |
| F33.3 | Major depressive disorder, recurrent, severe with psychotic symptoms |
| F33.41 | Major depressive disorder, recurrent, in partial remission |
| F33.42 | Major depressive disorder, recurrent, in full remission |
| F33.9 | Major depressive disorder, recurrent, unspecified |
The severity levels in F33 codes mirror those of F32. Additionally, these codes include a "Type 1 Excludes" note, meaning they cannot be used alongside codes for bipolar disorder (F31) or manic episodes (F30).
Related Codes for Depressive Disorders
Several depressive disorders related to MDD have distinct ICD-10 codes to ensure proper documentation:
- Dysthymia (Persistent Depressive Disorder): Coded as F34.1, this condition affects about 1.5% of American adults annually and is characterized by chronic, lower-grade depression.
- Postpartum Depression: Assigned F53.0, this condition impacts 10–15% of mothers each year and is distinct from the temporary "baby blues" that typically resolve within a week or two after childbirth.
- Seasonal Affective Disorder (SAD): Often coded as F33.9, this condition affects roughly 5% of Americans, with symptoms typically surfacing during the fall and winter months.
- Adjustment Disorders with Depressed Mood: Documented under F43.2, this applies when depressive symptoms arise in response to specific stressors but don’t meet the full criteria for MDD.
When assigning these codes, it’s important to evaluate personal and family history to distinguish depressive episodes from other mood disorders effectively.
Clinical Criteria and Documentation for MDD ICD-10 Codes
When documenting Major Depressive Disorder (MDD), it’s crucial to understand the clinical criteria that differentiate ICD-10 codes. Properly recording symptoms, their severity, and duration ensures accurate coding and compliance with healthcare standards.
Documenting Symptom Severity and Duration
According to ICD-10 guidelines, a diagnosis of MDD requires at least two core symptoms along with two additional symptoms. Similarly, the DSM-5 specifies five or more symptoms, including either a depressed mood or a loss of interest.
Severity levels – mild, moderate, or severe – are determined based on symptom count, intensity, and their impact on daily functioning. For accurate documentation, note the duration of symptoms, which must persist for at least two weeks, except in atypical cases with rapid onset. Chronic depression, on the other hand, requires symptoms to last for two or more years.
Be thorough when documenting how symptoms affect the patient’s work, social life, and daily activities. Tools like the PHQ-9 can help assess symptom severity and provide a structured way to support your documentation.
Detailed records like these are essential for tracking remission and progression, which we’ll explore next.
Recording Remission and Unspecified Presentations
When documenting remission, clarity is key. Full remission means symptoms are entirely absent, while partial remission indicates the persistence of minor symptoms. To distinguish between separate depressive episodes, ICD-10 requires documentation of at least two months without significant symptoms.
It’s also important to record the frequency of episodes and the patient’s current status concisely. Research shows untreated depressive episodes typically last six to eight months, with 80% of patients recovering within a year. However, many patients experience subthreshold depressive symptoms for extended periods. Accurately capturing these patterns informs both coding decisions and treatment plans.
Clear remission documentation not only supports accurate coding but also helps avoid common pitfalls in MDD documentation.
Common Mistakes in MDD Documentation
The Office of Inspector General has reported a 27% error rate in MDD diagnoses, emphasizing the need for precise documentation.
To avoid errors:
- Always include essential details like patient ID, provider signature, service times, and clear links between prescribed medications and diagnoses.
- Treatment plans should be specific – vague statements can lead to coding mistakes.
- Describe symptom severity with precision. For example, when coding a moderate single episode, explicitly state both the moderate severity and single episode status. Be sure to include all relevant characters in the ICD-10-CM code to reflect severity and clinical status accurately.
Avoid ambiguous terms like “history of” when describing active symptoms, as this could imply the condition has resolved rather than being ongoing. Focus instead on documenting current symptoms and their impact on the patient’s functioning.
Using structured formats like SOAP (Subjective, Objective, Assessment, Plan) notes can improve consistency, and detailing management steps – Monitor, Evaluate, Assess, Treat – ensures thorough documentation. Additionally, schedule follow-up visits within 12 weeks of starting new antidepressants and again at six months if treatment continues.
Best Practices for Accurate Documentation in the U.S.
Accurate documentation for Major Depressive Disorder (MDD) in the U.S. rests on three key pillars: adhering to regulatory standards, crafting clear clinical notes, and leveraging technology effectively. These elements form the backbone of precise and reliable documentation in clinical settings.
Complying with U.S. Regulatory Standards
The U.S. healthcare system enforces strict regulations to ensure uniformity in MDD documentation. Building on the ICD-10 framework, these rules promote consistency across healthcare environments. For example, HIPAA requires the use of national standards for electronic healthcare transactions, including diagnosis and procedure codes. The ICD-10-CM is the go-to standard for MDD diagnoses, playing a critical role in claims processing and reimbursement. However, it’s important to note that having a code doesn’t automatically guarantee payment or coverage.
Each year on October 1st, the Centers for Medicare & Medicaid Services (CMS) releases updated ICD-10-CM codes. Practices must adapt by updating their systems and training to stay compliant.
To ensure adherence to these standards, consider implementing written policies for handling external information requests and conducting regular audits of your coding practices. Every CPT code on a claim should be backed by an ICD-10 diagnosis code that establishes medical necessity. Make sure your progress notes clearly document the rationale for each service provided.
Writing Clear and Complete Clinical Notes
Strong clinical notes are the cornerstone of accurate MDD coding. These notes not only support patient care and communication but also fulfill legal and regulatory requirements. With the rise of open notes – where patients can access their records – there’s an even greater emphasis on writing high-quality documentation.
The best clinical notes are clear, concise, and thorough, offering enough detail to justify care decisions without unnecessary complexity. Following the "5 C’s" of documentation – clarity, conciseness, completeness, confidentiality, and chronological order – helps ensure accuracy and avoids potential legal or interpretative issues.
Using structured formats like SOAP (Subjective, Objective, Assessment, Plan) can improve note clarity. Incorporate objective data like PHQ-9 scores alongside patient-reported information, document observable facts, and use the patient’s own words when possible. Always tie interventions to treatment goals and use person-first, stigma-free language to maintain professionalism and empathy.
Timeliness is also key – aim to complete notes within 24–48 hours for accuracy. Dr. David Schillinger, Chief Medical Officer at SCP Health, emphasizes:
"Medical reimbursement is reflective of what you document, not just what you do".
Avoid using jargon or abbreviations that could confuse readers, especially as open notes are now the norm. Write in a way that addresses patient concerns, use supportive language, and always date and sign your notes. For confidentiality, apply the "Minimum Necessary" rule and encourage patients to review their notes, providing feedback when appropriate.
Using Technology for Efficient Documentation
While well-written clinical notes are essential, technology can take documentation to the next level. Advanced tools ensure consistency in format and capture critical details like symptom duration, severity, and functional impact – key elements for accurate ICD-10 coding.
Real-time validation features in electronic health records (EHRs) can detect errors instantly, such as missing details or vague descriptions, allowing providers to correct issues during the patient encounter. This proactive approach helps avoid problems that might otherwise surface during billing reviews.
Additionally, smart documentation systems automatically update ICD-10-CM codes when CMS releases new versions each October 1st. These systems can notify providers of any changes that might affect MDD documentation, ensuring compliance and reducing the risk of errors.
sbb-itb-5a50404
Improving MDD Documentation with DocScrib

DocScrib’s AI-powered platform tackles the challenges of documenting Major Depressive Disorder (MDD), a condition often overlooked or misdiagnosed. With two-thirds of MDD cases in the U.S. remaining undiagnosed or unspecified, precise documentation is critical for both effective patient care and meeting regulatory standards.
DocScrib Features for MDD Coding
DocScrib streamlines MDD documentation with a variety of tools tailored to mental health care:
- Real-time transcription: Captures patient conversations as they happen, ensuring no detail is missed. The platform’s AI understands mental health terminology and organizes the data according to ICD-10-CM guidelines for MDD.
- Customizable templates: These templates incorporate tools like PHQ-9 and SIGECAPS for documenting symptom severity, duration, and impact. Using the SIGECAPS mnemonic (Sleep, Interest, Guilt, Energy, Concentration, Appetite, Psychomotor, Suicidality), providers can ensure all relevant symptoms are recorded.
- EHR integrations: DocScrib can pull data from existing patient records, helping providers differentiate between single episodes (F32 codes) and recurrent episodes (F33 codes) of depression. It also tracks SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound) within treatment plans, making it easy to document progress and adjust codes as needed.
- Analytics dashboard: This feature highlights trends and gaps in documentation, helping practices improve MDD coding accuracy. Given that routine outcome tracking can reduce patient deterioration rates by 50%, this capability supports both better patient outcomes and improved coding reliability.
By combining these features, DocScrib not only boosts coding accuracy but also simplifies clinical workflows.
How DocScrib Improves Workflow Efficiency
DocScrib’s automation significantly reduces the burden of documentation, allowing clinicians to dedicate more time to patient care. The platform automatically records encounters in real time, which is particularly helpful in mental health settings where maintaining eye contact and building rapport are vital.
The AI system ensures thorough documentation by noting both the presence and absence of symptoms during each session. This is essential for tracking patient progress and justifying ongoing treatment. Additionally, it prompts providers to address key indicators of depression without disrupting the natural flow of conversation.
Collaboration is seamless with DocScrib’s multi-user access feature. For example, a nurse can document initial PHQ-9 screening results, while the physician adds clinical assessments and treatment plans. This shared approach ensures complete records while distributing the workload.
To further support efficiency, DocScrib offers priority support to quickly resolve technical issues and custom workflows that cater to each practice’s preferred documentation style, whether it’s SOAP notes or another format.
Pricing Plans for Different Practice Needs
DocScrib offers flexible pricing to suit practices of all sizes, ensuring that providers can access the tools they need without overpaying for unnecessary features:
| Plan | Monthly Cost | Patient Visits | Key MDD Features | Best For |
|---|---|---|---|---|
| Starter | $49 | Up to 100 | Basic note templates, real-time transcription, HIPAA-compliant storage | Solo practitioners, part-time providers |
| Professional | $99 | Up to 500 | AI-powered notes, custom templates, analytics, multi-user access (up to 3 users) | Small to medium practices, group therapy |
| Enterprise | Custom pricing | Unlimited | Custom AI training, dedicated account manager, 24/7 priority support, analytics | Large practices, hospitals, integrated networks |
The Starter plan is ideal for solo providers with a manageable patient load. At $49 per month, it offers essential tools like real-time transcription and HIPAA-compliant storage without unnecessary extras.
For $99 per month, the Professional plan adds features like an analytics dashboard and multi-user access, making it a great fit for group practices. This plan is particularly useful for tracking depression screening rates and ensuring documentation completeness. With 30% of patients reporting depressive symptoms but fewer than 10% diagnosed with major depression, these tools are invaluable.
The Enterprise plan is tailored to the needs of larger organizations. It includes custom AI model training to align with specific documentation styles and terminology, as well as a dedicated account manager for smooth implementation and ongoing support.
All plans prioritize HIPAA-compliant data security and integrate screening tools like PHQ-9 into annual wellness exams. This is especially important given the 27.6% increase in major depression cases during the COVID-19 pandemic, highlighting the need for systematic screening and thorough documentation.
Conclusion: Improving MDD Documentation Standards
Key Points Summary
Getting the ICD-10 coding right for Major Depressive Disorder (MDD) is more than just a technical task – it’s a cornerstone for effective patient care, thoughtful treatment planning, and impactful clinical research. The level of detail in your documentation plays a direct role in shaping patient outcomes and ensuring the long-term viability of your practice.
When documenting MDD, make sure to capture every depressive episode and its severity with the most accurate ICD-10 code available. Use the most specific code that aligns with your clinical documentation. Your records should include all critical patient data, clear and concise notes, and verified provider credentials. This thoroughness helps avoid coding errors and any complications that might arise from them.
The Cleveland Clinic demonstrated the power of improved documentation through a human-assisted AI approach, which led to a 15% boost in case-mix index accuracy and a 30% drop in retrospective queries.
"We’re really not taking care of records; we’re taking care of people. . . . This record cannot be separated from the caring of that patient. . . . This is the practice of medicine."
– Dr. Larry Weed, Founder of SOAP Notes
These lessons provide a roadmap for practical improvements.
Next Steps for Clinicians
To act on these insights, start with a few tangible steps. Develop a quick-reference guide for commonly used behavioral health codes and make it a habit to conduct regular chart audits to check for coding accuracy. Stay informed about annual ICD-10-CM updates, and focus on key documentation principles: accuracy, completeness, consistency, precision, timeliness, and legibility.
Consider integrating AI-powered tools into your documentation process. These tools can work with your existing EHR system to autocomplete diagnosis fields, suggest appropriate codes based on clinical notes, and streamline communication with billing teams. They can also turn unstructured clinical data into actionable insights while maintaining HIPAA compliance.
"If we put our heads together, those of us with a clinical background and those with an informatics background can come together and really achieve that vision of reducing documentation by 75% by 2025."
– Christine Sinsky, MD, AMA Vice President of Professional Satisfaction
Encourage collaboration between clinicians and documentation specialists, and implement ongoing training programs to stay aligned with best practices and regulatory requirements.
FAQs
How do I choose the correct ICD-10 code for different levels of Major Depressive Disorder?
To choose the right ICD-10 code for Major Depressive Disorder (MDD), it’s important to match the code to the specific severity and clinical details of the condition. Here are some examples:
- F32.1: Represents a moderate depressive episode.
- F32.2: Indicates a severe depressive episode without psychotic features.
- F32.3: Refers to a severe depressive episode with psychotic features.
- F33.2: Used for a recurrent severe depressive episode.
Always consult the most recent ICD-10 coding guidelines to ensure accuracy and compliance. Detailed documentation of symptoms and clinical findings is essential for selecting the correct code.
What are the key mistakes to avoid when documenting Major Depressive Disorder (MDD) to stay compliant with healthcare standards?
Avoiding Common Errors in Documenting MDD
When documenting Major Depressive Disorder (MDD), it’s important to steer clear of these frequent mistakes:
- Not specifying symptom duration: Symptoms must last at least two weeks to meet the diagnostic criteria.
- Failing to note severity: Be sure to document whether the condition is mild, moderate, or severe.
- Missing core symptoms: Always include key indicators such as depressed mood or loss of interest/pleasure (anhedonia).
- Neglecting to rule out other causes: Ensure symptoms are not due to medical conditions or substance use.
Thorough and precise documentation not only ensures compliance but also supports accurate coding and promotes better outcomes for patient care.
Why is accurate ICD-10 coding for Major Depressive Disorder important for insurance claims and patient care?
Accurate ICD-10 coding for Major Depressive Disorder (MDD) plays a critical role in ensuring insurance claims are processed smoothly and without unnecessary denials. By clearly conveying the severity and specifics of a patient’s condition to insurers, proper coding helps cut down on administrative headaches and delays.
Beyond insurance, precise coding is also key to crafting effective treatment plans. It provides a detailed clinical snapshot that aligns with documentation standards, paving the way for care decisions tailored to the patient’s needs. This level of clarity can make a real difference in improving patient outcomes.