Updated on: July 5, 2025
In the fast-paced world of healthcare, accurate and timely documentation is essential for effective patient care. Progress notes are the cornerstone of clinical communication, providing an ongoing record of a patient’s status, treatment, and response. In this comprehensive guide, we’ll explore the types of progress notes, their formats, real-world examples, and how innovative tools like AI medical scribes can streamline the documentation process.
What Are Progress Notes?
Progress notes are essential clinical documents that capture the patient’s journey during their care episodes. They record observations, assessments, interventions, and patient responses, ensuring continuity across healthcare providers and departments.
Progress notes serve various purposes:
- Facilitate communication between healthcare team members
- Provide legal documentation of care
- Support billing and coding
- Improve patient safety and outcomes
Why Are Progress Notes Important?
- Clinical Communication: Ensure seamless information flow across providers.
- Legal Protection: Serve as legal evidence of care provided.
- Billing & Compliance: Meet regulatory and reimbursement requirements.
- Continuity of Care: Help track patient progress over time.
Common Types of Progress Notes in Healthcare
There are multiple formats used for documenting progress notes, each tailored to specific clinical settings or specialties. Here’s a breakdown of the most widely used types:
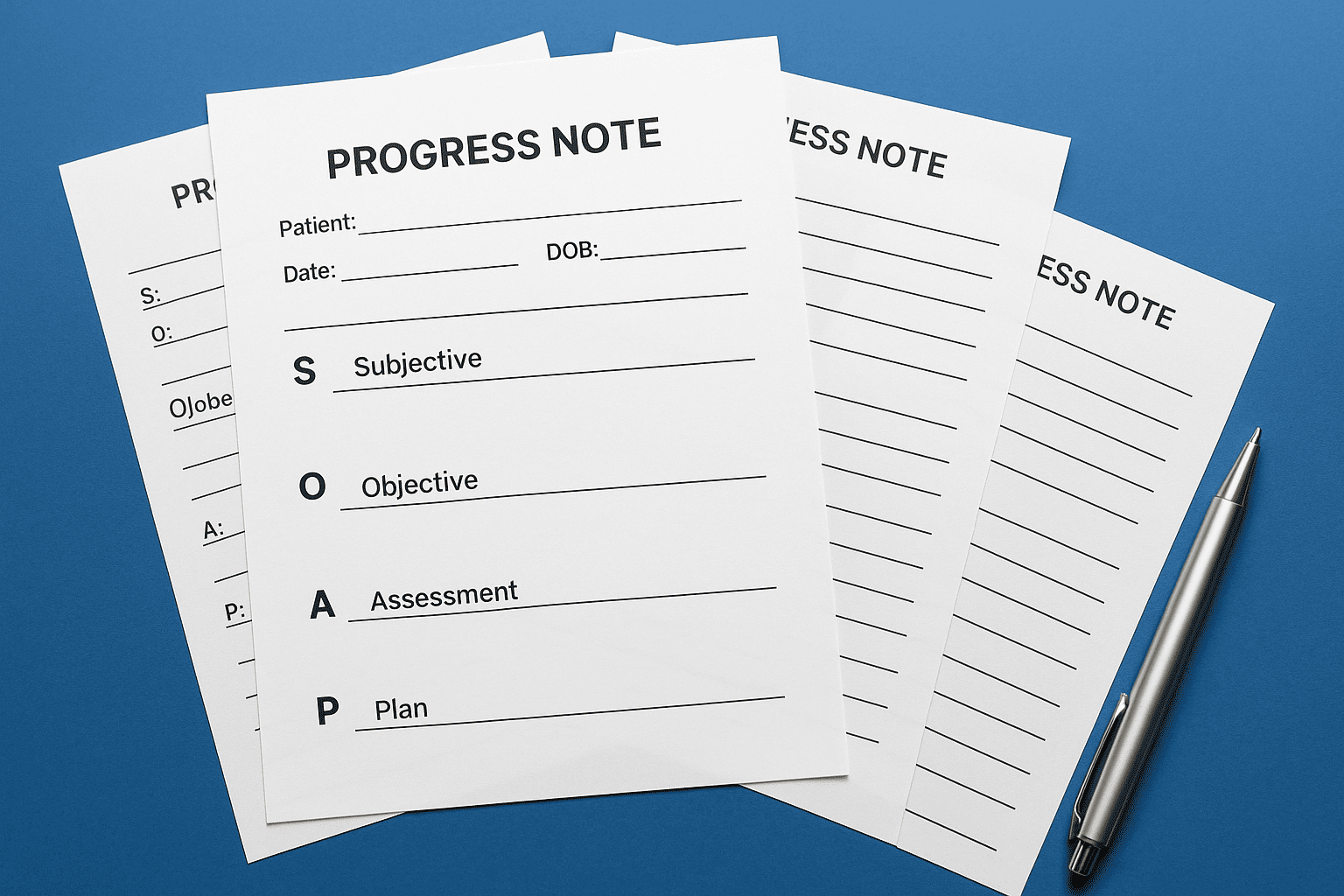
1. SOAP Notes (Subjective, Objective, Assessment, Plan)
Overview: SOAP notes are the most common progress note format in healthcare. They follow a structured approach:
- Subjective: Patient’s reported symptoms or concerns
- Objective: Measurable, observable clinical findings
- Assessment: Clinician’s interpretation or diagnosis
- Plan: Next steps in treatment or care
Example: Subjective: Patient reports increased shortness of breath over past two days. Objective: Respiratory rate 24, O2 sat 93% on room air. Assessment: Exacerbation of COPD. Plan: Start nebulizer therapy, follow-up in 2 days.
2. DAP Notes (Data, Assessment, Plan)
Overview: DAP notes are widely used in behavioral health and counseling settings.
- Data: Subjective and objective observations
- Assessment: Clinician’s interpretation
- Plan: Interventions and follow-up
Example: Data: Patient appeared anxious, fidgeting throughout session. Assessment: Ongoing anxiety related to work stress. Plan: Teach deep breathing techniques, schedule next appointment.
3. BIRP Notes (Behavior, Intervention, Response, Plan)
Overview: BIRP notes are primarily used in mental health, especially in psychiatric settings.
- Behavior: Patient’s behaviors or statements
- Intervention: Clinician’s action
- Response: Patient’s reaction
- Plan: Next steps
Example: Behavior: Patient expressed feelings of hopelessness. Intervention: Provided cognitive restructuring techniques. Response: Patient engaged well, expressed willingness to practice. Plan: Continue CBT-focused sessions.
4. PIRP Notes (Problem, Intervention, Response, Plan)
Overview: Similar to BIRP, PIRP focuses more on problem identification and management.
Example: Problem: Persistent insomnia despite medication. Intervention: Discussed sleep hygiene strategies. Response: Patient willing to trial new bedtime routine. Plan: Monitor progress over next two weeks.
5. IER Notes (Intervention, Evaluation, Response)
Overview: IER notes are streamlined for documenting therapeutic interventions.
Example: Intervention: Guided relaxation exercise. Evaluation: Patient remained calm and receptive. Response: Reported reduced anxiety levels.
How AI Medical Scribes Like DocScrib Simplify Progress Notes
Healthcare providers often face the challenge of balancing patient care with the time-consuming demands of documentation. That’s where AI medical scribes like DocScrib come in.
Benefits of Using AI Medical Scribes:
- Time-Saving: Automates note creation, reducing documentation burden.
- Consistency: Ensures standardized note formats like SOAP, DAP, or BIRP.
- Accuracy: Minimizes human error by capturing detailed information.
- Compliance: Helps meet HIPAA and billing regulations.
Real-World Applications:
- Primary Care
- Psychiatry
- Physical Therapy
- Telemedicine
Want to experience the future of clinical documentation? Schedule a Demo with DocScrib
How to Choose the Right Progress Note Format
Choosing the correct progress note format depends on:
- Clinical Setting: Mental health, primary care, rehab, etc.
- Compliance Needs: Legal and insurance requirements.
- Team Preferences: Organizational guidelines or EHR templates.
Tips for Writing Effective Progress Notes
- Be Concise but Comprehensive
- Use Clear, Non-Jargon Language
- Document Only Relevant Information
- Maintain Objectivity
- Leverage AI Tools like DocScrib for Efficiency
Frequently Asked Questions (FAQs)
Q1. What is the most common type of progress note? A1. The SOAP note is the most widely used progress note format in healthcare settings.
Q2. Are AI medical scribes HIPAA-compliant? A2. Yes, trusted solutions like DocScrib are designed to meet HIPAA standards.
Q3. Can AI scribes write different types of progress notes? A3. Absolutely. Tools like DocScrib can generate SOAP, DAP, BIRP, and more.
Q4. How can I reduce time spent on documentation? A4. Using an AI medical scribe like DocScrib significantly reduces documentation time and frees you to focus on patient care.
Conclusion
Accurate and efficient progress note documentation is key to high-quality patient care, clinical compliance, and professional communication. By understanding the different types of progress notes—from SOAP to BIRP—you can choose the right format for your setting. And with AI medical scribes like DocScrib, you can simplify this process while maintaining accuracy, speed, and compliance.
Ready to streamline your clinical documentation? Book a personalized demo with DocScrib today!