Updated on: July 20, 2025
SOAP notes are a structured way for speech-language pathologists (SLPs) to document therapy sessions, ensuring clear communication, compliance, and progress tracking. They consist of four sections: Subjective (client’s perspective), Objective (measurable data), Assessment (professional interpretation), and Plan (next steps). Properly written SOAP notes not only meet professional and legal standards but also improve collaboration, clarify goals, and support insurance claims. For SLPs managing heavy workloads, tools like DocScrib can simplify documentation with real-time transcription and customizable templates, saving time and reducing stress.
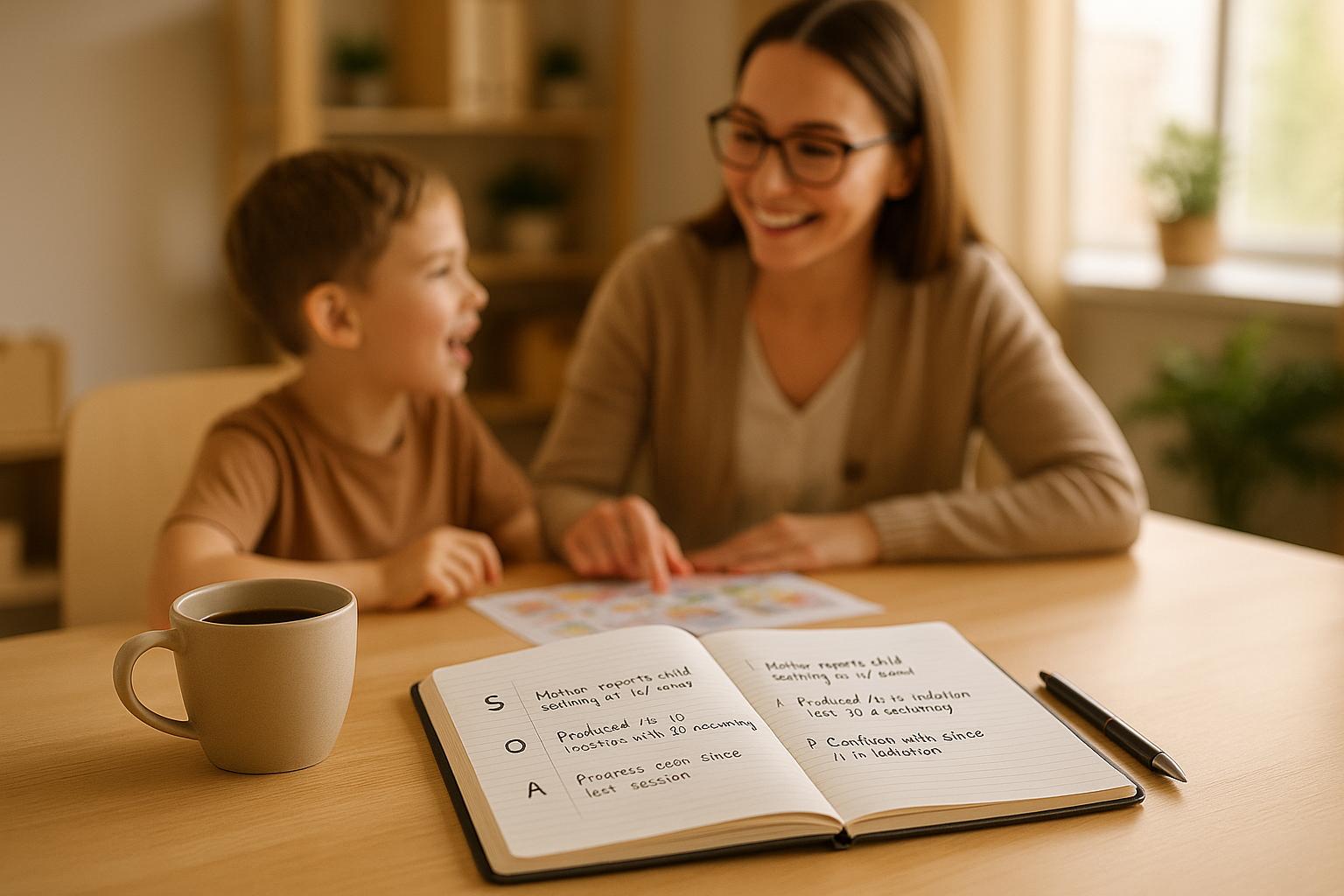
SOAP Notes for Speech Therapy
Understanding the 4 Parts of SOAP Notes
Each component of a SOAP note serves a distinct purpose in documenting a session. When structured properly, these notes ensure thorough and professional records. Let’s break down the key aspects of each section to help you create effective documentation.
Subjective: Recording Client Perspectives
The subjective section focuses on the client’s own words and experiences. This is where you document what the client shares about their challenges, progress, or concerns. It’s all about capturing their perspective – how they feel, what they’ve noticed, and their perceptions.
Whenever possible, use direct quotes to preserve the client’s voice. For instance, instead of summarizing with "Client seemed anxious", you might write: "Client reports feeling more anxious this week. She described feeling jittery, on edge, and noted an increase in anxious thoughts".
This section can also include input from caregivers when relevant, providing a fuller picture of the client’s experiences and challenges.
Objective: Recording Measurable Data
In the objective section, you focus on observable, measurable facts. This is where you document what you, as the clinician, directly observed during the session. It might include test results, task performance, or physical behaviors.
For example, a detailed entry could read: "Johnny produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal met for 2 out of 3 consecutive sessions)".
You can also include observations about the client’s demeanor or behavior, such as: "During the session, the client was fidgety, wringing her hands, and speaking quickly. She appeared to have difficulty concentrating".
Assessment: Interpreting Therapy Progress
This section is where you analyze the information gathered in the subjective and objective sections. It’s your professional interpretation of the client’s progress and response to therapy.
For instance, in the case of a school-age child working on stuttering, you might write: "The client shared more communication situations than previously and spoke with confidence about their plan. Role-playing is a favorite activity, and the client is demonstrating less fear about what others might think. Independent use of pseudo-stuttering was new and reflects increased comfort and confidence".
For an adult in voice therapy, an assessment might look like this: "The client met goals of optimal voicing to meet vocational demands, as evidenced by an improvement from vocal effort of 7/10 (‘somewhat hard’) to 4/10 (‘somewhat easy’). Progress is evident in carryover of SOVT strategies to social contexts".
Plan: Structuring Next Steps
The plan section outlines the roadmap for the client’s continued care. This includes therapy goals, strategies, and any changes to the current approach. Goals should be realistic and measurable, following the SMART framework – Specific, Measurable, Achievable, Realistic, and Time-Bound.
For example, in a preschool articulation session, you might write: "Send a list of words with /k/ in the initial position to the client’s mother, along with instructions on using carrier phrases during play. Introduce visual cues to support generalization and reduce reliance on phonemic cues".
Keep the plan focused and actionable. Tie goals directly to the issues identified in the assessment, and avoid overwhelming the client with too many objectives. Include specific next steps, like scheduling, referrals, or home activities, to ensure clarity and follow-through.
Best Practices for Writing SOAP Notes
Writing effective SOAP notes goes beyond understanding their four-part structure. The quality of your documentation depends on applying clear writing principles and following established standards. Well-crafted SOAP notes not only safeguard you and your clients but also ensure seamless communication within the care team.
Maintaining Clarity and Consistency
Keep your language straightforward. Avoid using overly technical terms that might confuse other professionals or family members reviewing the notes. For instance, instead of saying, "Client exhibited dysfluent speech patterns", opt for something like, "Client stuttered on 15% of words during conversation." This makes your observations easier to understand for everyone involved.
Be specific and measurable. Replace vague phrases like "good progress" with precise data, such as "accuracy improved from 60% to 85% over three sessions." When describing behaviors, focus on concrete examples rather than subjective interpretations. For example, write "Client looked away during 8 out of 10 questions" instead of "Client seemed uncooperative."
"Clear, consistent, and concise notes ensure accessible communication for therapists, caregivers, and insurers." – TheraPlatform
Use templates and standardized formats for efficiency. A consistent structure for each section, coupled with clear headings, makes your notes more organized. Bullet points can help when listing multiple observations or goals, ensuring no important details are missed.
Stick to consistent terminology. Using the same terms (e.g., always referring to "phonemic awareness") ensures clarity and professionalism. Establish a list of preferred abbreviations and terms to maintain uniformity across all documentation.
Following US Documentation Standards
Clear writing is just one part of effective SOAP notes – meeting legal requirements is equally critical. SOAP notes are legal documents and may be used in court proceedings. This underscores the importance of documenting care accurately and thoroughly. Incomplete or unclear records could result in reimbursement denials or legal issues.
Include essential details like patient identifiers, date/time stamps, signatures, and credentials. Never backdate or erase entries. If corrections are needed, add amendments with proper dates and initials to maintain the integrity of the documentation.
Ensure HIPAA compliance when handling client information. Use encrypted platforms for storing and sharing digital SOAP notes. Avoid discussing client details in public or using unsecured communication methods to protect privacy.
Document medical necessity and skilled interventions clearly. Explain why therapy services are needed and provide a rationale for your treatment decisions.
Follow state and federal regulations. Each state has specific laws for medical record retention, and licensing boards require healthcare professionals to maintain legible, timely, and legally sound documentation. Always adhere to the most stringent applicable standard and stay updated on the requirements in your region.
Avoiding Common Documentation Errors
Inconsistencies in documentation can lead to confusion and legal risks. Regular training and monitoring help ensure adherence to clinic standards for terminology, abbreviations, and formatting.
Delays in documenting changes can jeopardize client care. Establish clear policies requiring immediate updates to treatment plans, goals, or client status. When immediate documentation isn’t feasible, implement a system to record key details for later entry.
"If it wasn’t documented, it wasn’t done." – American Speech-Language-Hearing Association (ASHA)
Incomplete notes create gaps in treatment continuity. Make sure every SOAP note includes all four sections with relevant details. Missing signatures or incomplete consent forms can pose both clinical and legal challenges.
Avoid vague terms and provide measurable details. Replace words like "improved" or "better" with specific percentages or detailed observations that other professionals can reference.
Base statements on direct observations or client comments. For example, instead of writing "Client seems frustrated", document "Client stated, ‘This is really hard and I don’t think I’m getting better.’"
Avoid redundancy across sections. Each part of the SOAP note has a distinct purpose. Use the assessment to analyze information from the subjective and objective sections, and let the plan focus on actionable next steps.
sbb-itb-5a50404
Improving SOAP Notes with DocScrib

Using AI to improve SOAP notes aligns with the broader goal of creating clear and efficient clinical documentation for speech-language pathologists (SLPs). For SLPs managing a heavy caseload, balancing detailed documentation with patient care can be overwhelming. DocScrib’s AI-powered platform tackles this challenge by reducing paperwork while maintaining high standards for quality and compliance.
Research shows that clinicians spend nearly 50% of their workday on documentation tasks. For SLPs, this workload often extends beyond clinic hours, cutting into personal time. DocScrib changes the game by automating much of the documentation process, allowing clinicians to focus on patient care without sacrificing accuracy. Let’s explore the features that make DocScrib a valuable tool for SOAP note creation.
Features Supporting SOAP Note Creation
DocScrib offers real-time transcription that captures spoken interactions during sessions and converts them into structured SOAP notes. This means SLPs can stay fully engaged with their clients while the AI handles the documentation in the background.
Customizable templates designed specifically for speech therapy streamline the SOAP process. These templates ensure all key sections – Subjective, Objective, Assessment, and Plan – are organized and completed. By auto-populating relevant fields based on the session content, the platform reduces the need for manual input, saving time and effort.
DocScrib also prioritizes security with HIPAA-compliant storage and enterprise-grade protections for sensitive client data. The platform integrates seamlessly with major EHR systems like Epic, Cerner, and Athenahealth, ensuring smooth workflows and compliance with federal privacy standards.
Additional features like coding suggestions and EHR export options simplify billing and record-keeping. This ensures that documentation supports reimbursement requirements while remaining clinically accurate.
"At DocScrib, we build on this AI dictation revolution: our platform supports ambient capture, structured templates, coding suggestions, and EHR exports – all within a secure, compliant environment. Providers retain ultimate control, while AI handles heavy-lifting behind the scenes." – DocScrib
Adding DocScrib to Clinical Workflows
DocScrib integrates easily into existing clinical workflows without disrupting routines. SLPs can start using the platform right away, as the AI operates in the background. Clinicians simply speak naturally during sessions, and the system takes care of the rest.
A pilot program is a great way to refine the workflow and tailor the AI to match specific documentation preferences. The recommended approach involves letting the AI draft the notes, followed by clinician review to ensure accuracy before finalizing. This process reduces documentation time while keeping clinicians in control of their work.
By cutting documentation time by up to 50%, DocScrib can save SLPs 2–3 hours each day. For clinicians managing multiple clients, this means completing documentation during clinic hours instead of taking work home.
Dr. Sharma, a pediatrician who uses DocScrib, shared her experience:
"Before adopting DocScrib, I was spending nearly two hours each evening finishing my notes. Now, my documentation is done before I leave the clinic. My patients feel heard, and I feel less stressed." – Dr. Sharma, Pediatrician
| Feature | DocScrib | Manual Charting |
|---|---|---|
| Real-time documentation | ✅ Yes | ❌ No |
| Auto-populated templates | ✅ Yes | ❌ No |
| Time saved per shift | ✅ Up to 3 hours | ❌ None |
| Reduces burnout | ✅ Significant | ❌ No |
With its seamless integration and proven efficiency, DocScrib offers flexible pricing plans designed to meet the needs of various practice sizes.
DocScrib’s Pricing and Plans
DocScrib provides three pricing tiers to suit different practice needs, each offering core features for SOAP note creation. These plans scale to accommodate individual practitioners as well as large clinical teams, ensuring flexibility and efficiency.
- Starter Plan: Priced at $49 per month, this plan is ideal for individual practitioners. It includes support for up to 100 patient visits monthly, real-time transcription, basic clinical note templates, HIPAA-compliant storage, and standard EHR integrations.
- Professional Plan: At $99 per month, this plan is tailored for busy practitioners and small clinics with higher documentation demands. It supports up to 500 patient visits monthly and includes advanced AI-powered notes, a custom template library, priority support, and an analytics dashboard. Multi-user access for up to three users makes it a great fit for small teams.
- Enterprise Plan: Custom-priced for large practices or health systems, this plan offers unlimited patient visits and advanced features. It includes enterprise-grade security, custom AI model training, dedicated account management, and 24/7 priority support. Large teams benefit from unlimited users, advanced analytics, and on-premise deployment options.
DocScrib’s flexible pricing allows practices to start small and expand as they experience the benefits of AI-powered documentation.
Conclusion: Better Documentation with SOAP Notes
SOAP notes play a critical role in speech therapy by providing a clear and structured way to document client interactions, monitor progress, and meet compliance requirements in the U.S.
The four-part SOAP framework – discussed earlier – ensures documentation that is consistent and precise. This structure not only improves communication between providers but also strengthens clinical assessments and creates a solid foundation for reimbursement claims.
When tools like DocScrib come into play, the documentation process becomes far less time-consuming. Manual charting, which often eats up hours, can be streamlined with features like real-time transcription and customizable templates. These tools can cut documentation time by up to 50%, giving clinicians more time to focus on their clients.
There’s also a financial upside to efficient documentation. Clinicians using digital tools have reported saving over $3,500 per month on administrative costs. Beyond the savings, thorough SOAP notes help ensure compliance, support reimbursement claims, and protect against legal risks – all while contributing to measurable clinical progress.
FAQs
How do SOAP notes help speech-language pathologists collaborate with other healthcare providers?
SOAP notes serve as a clear and organized method for recording patient progress, treatment strategies, and clinical insights. This format enables speech-language pathologists (SLPs) to effectively share critical information with other healthcare professionals, including doctors, occupational therapists, and physical therapists.
With their structured approach, SOAP notes ensure that updates are communicated consistently, helping to build a collaborative care plan that aligns with the patient’s broader health objectives. This approach minimizes misunderstandings, enhances teamwork, and supports better results for the patient.
What mistakes should SLPs avoid to create effective and compliant SOAP notes?
Writing Effective SOAP Notes for SLPs
To make SOAP notes both effective and compliant, it’s crucial for SLPs to steer clear of common mistakes. Avoid using vague or overly subjective language, as well as making broad generalizations without evidence. Instead, focus on being specific – use objective data to support your observations and steer clear of ambiguous phrases, especially when describing symptoms reported by patients.
Timeliness is also key. Writing notes promptly and including relevant details about progress or changes in therapy helps maintain accuracy. Clear and precise documentation not only ensures compliance but also provides a reliable way to track therapy goals over time.
How can DocScrib help Speech-Language Pathologists create more accurate and efficient SOAP notes?
DocScrib simplifies the process of creating SOAP notes for Speech-Language Pathologists (SLPs) by automating essential tasks. This reduces the chance of errors from manual entry and ensures that notes are well-organized, clear, and consistent. The result? Less time spent on paperwork and better alignment with clinical standards.
With its structured approach, DocScrib allows SLPs to dedicate more attention to their patients rather than administrative duties, improving the accuracy of documentation and streamlining daily workflows.