Updated on: July 19, 2025
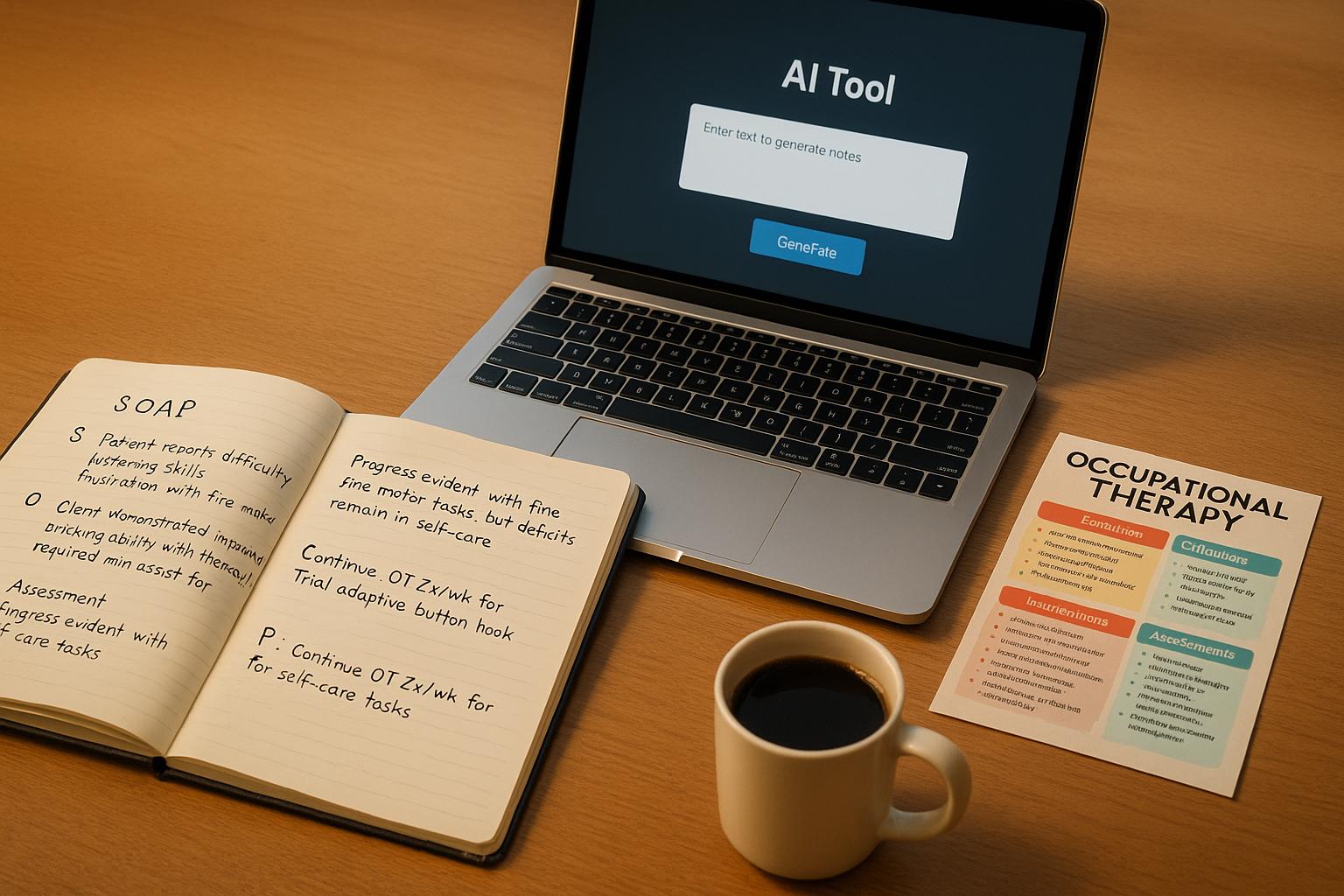
SOAP notes are a cornerstone of occupational therapy documentation, offering a structured way to record patient care. This format – Subjective, Objective, Assessment, and Plan – ensures clear, consistent, and measurable notes that guide treatment and support compliance with U.S. healthcare standards. Proper documentation improves patient outcomes, reduces errors, and supports insurance claims.
Key takeaways from this article:
- SOAP Note Breakdown:
- S (Subjective): Patient-reported experiences (e.g., pain levels).
- O (Objective): Measurable data (e.g., range of motion, task performance).
- A (Assessment): Therapist’s professional evaluation.
- P (Plan): Next steps for care.
- Examples:
- Adult cases (e.g., wheelchair mobility, post-surgery hand therapy).
- Pediatric cases (e.g., handwriting, anxiety management).
- AI Tools like DocScrib simplify documentation:
- Real-time transcription.
- Customizable templates.
- HIPAA compliance.
- EHR integration.
- Cheat Sheets for Efficiency:
- Common abbreviations (e.g., ADL, ROM, MMT).
- Measurement conversions (e.g., inches to cm).
- Assessment tools (e.g., COPM, FIM, TUG).
- Tips for Better Notes:
- Write immediately after sessions.
- Be specific and measurable.
- Link interventions to goals.
- Avoid vague or repetitive language.
Accurate SOAP notes not only streamline workflows but also enhance patient care and compliance. Tools like DocScrib can save time and reduce burnout, helping therapists focus on what matters most: their patients.
OT Potential Documentation Examples: Your OT SOAP Note Help
SOAP Note Examples for Occupational Therapy
Real SOAP note examples provide a clear look at effective documentation practices. These examples follow proper structure while meeting U.S. healthcare standards and insurance requirements.
Adult OT SOAP Note Examples
Adult occupational therapy often focuses on rehabilitation after injuries, surgeries, or managing chronic conditions. Here are two examples showcasing detailed documentation techniques.
Wheelchair Mobility Training Case
This case highlights adaptive equipment modifications and functional improvements:
S: "Patient states she has been unable to use her wheelchair around her home because ‘my hands are hurting’ and ‘I am not able to get a good grip.’ Reports feeling overwhelmed by the challenges of independent mobility."
O: "OT assessed wheelchair and modified it by building up the rims with self-adhesive tape. Patient was instructed in techniques for propelling wheelchair over carpet and thresholds safely. Following adaptation, patient demonstrated ability to self-propel 100 feet with minimal verbal cues while reporting 0/10 hand pain."
A: "After wheelchair adaptation and instruction, patient showed marked improvement in self-propulsion capabilities and increased independence in functional mobility within the home environment. Patient demonstrates high motivation to regain independence and responds well to instructions."
P: "Patient will benefit from continued skilled OT intervention focusing on wheelchair mobility down ramps to access the living area. Will acquire ultra-grip built-up rim covers for trial at the next visit as a potential long-term solution versus temporary tape modification."
Hand Therapy Post-Surgery Case
This example involves a software engineer recovering from carpal tunnel release surgery:
S: "Patient is a right-handed male software engineer who states he had a severe increase in pain and tingling in his right hand, which led to right carpal tunnel release surgery on 11/30/24. He presents to OT with complaints of pain and residual stiffness while performing typing movements, stating, ‘I’m supposed to go back to work in three weeks, and I don’t know how I will be able to function with this pain.’ Post surgery, patient complains of 2/10 pain at rest and 7/10 shooting pain at the palmar region extending to the second and third digits of the right hand when working at his computer for extended periods and when performing basic household chores such as carrying heavy objects (like laundry and groceries). The numbness and tingling experienced prior to surgery have resolved dramatically."
O: "Range of motion and strength:
Left upper extremity: Range of motion within functional limits at all joints and on all planes.
Right upper extremity: Right shoulder, elbow, forearm, and digit range of motion all within normal limits on all planes.
Right wrist:
• Flexion/extension – Strength: 4/5, AROM: 50/50, PROM: 60/60
• Radial/ulnar deviation – Strength: 4/5, AROM: within normal limits, PROM: not tested.
Standardized assessments:
• Dynamometer – Left hand: 65/60/70; Right hand: 45/40/40
• Boston Carpal Tunnel Outcomes Questionnaire (BCTOQ) – Symptom Score = 2.7, Functional Score = 2.4
Sutures were removed and the wound is healing well with some edema, surgical glue, and scabbing remaining. Patient was provided education regarding ergonomic setup at work and home, along with a home exercise program that includes active digital flexor tendon gliding, wrist flexion and extension, active thumb opposition, active isolated flexor pollicis longus glide, and passive wrist extension (to be completed 4–6 times per day, 5–10 repetitions each). Patient was able to verbally repeat the home exercise program, demonstrated the exercises for the therapist, and was given a handout. Additionally, he received verbal and written instructions in scar management techniques and scar mobilization massage (3 times/day for 3–5 minutes) and was issued a scar pad to be worn overnight with a tubular compression sleeve."
A: "Mr. Peppercorn is a 46-year-old male who presents with decreased right grip strength and range of motion, as well as persistent pain following carpal tunnel release surgery. These deficits negatively impact his ability to write, type, and manipulate his laptop and door handles. Although his progress may be slower initially due to diabetes, his Boston Carpal Tunnel Outcomes Questionnaire scores indicate he is not progressing as expected and he is at risk of being among the 10–30% of patients who do not achieve positive outcomes following carpal tunnel release. Patient will benefit from skilled OT to address these deficits, adhere to the post-op treatment protocol, and return to work on light duty for the first four weeks."
P: "Recommend skilled OT services 1×/week consisting of therapeutic exercises, therapeutic activities, ultrasound, phonophoresis, e-stim, hot/cold therapy, and manual techniques. The services will target deficits in grip strength and range of motion as well as right hand pain.
Short Term Goals (2 weeks):
• Patient will increase dynamometer scores in both hands to 75 lb to manage daily tasks such as laundry.
• Patient will increase right digit strength to 3+/5 to open door handles without needing left hand support.
Long Term Goals (6 weeks):
• Patient will increase right wrist strength to 5/5 to facilitate carrying groceries.
• Patient will achieve an active range of motion in the wrist within normal limits to handle laptop and door operations without increased pain.
• Patient will increase bilateral hand dynamometer scores to 90 lb to return to recreational activities, with a corresponding decrease in his BCTOQ scores to less than 1.7 on both symptoms and function, allowing a return to work and social activities without restrictions."
Pediatric OT SOAP Note Examples
Pediatric cases often revolve around developmental and academic challenges. Here are two examples tailored for younger patients.
School-Based Handwriting Intervention
This case focuses on a student struggling with fine motor skills and handwriting endurance:
S: "Student reports hand fatigue after writing a three-page essay, stating they had a ‘rough day’ during writing tasks. The teacher notes increased avoidance of written assignments and frequent requests for breaks during handwriting activities."
O: "Student participated in a 30-minute session focused on handwriting and fine motor exercises. The observation revealed decreased grip strength in the dominant hand and inconsistent letter formation. The writing sample showed irregular spacing and variations in letter size. Student completed fine motor activities with moderate assistance and required frequent rest breaks every 5 minutes during writing tasks."
A: "Student exhibits signs of fine motor weakness affecting handwriting endurance and quality, which in turn impacts academic performance and classroom participation. The student responds well to structured breaks and demonstrates motivation to improve writing skills."
P: "Continue the current handwriting intervention plan with an emphasis on building fine motor strength and endurance. Teach strategies to manage hand fatigue during extended writing sessions, including scheduled breaks and grip-strengthening exercises, and collaborate with the teacher to implement classroom accommodations."
Anxiety Management for Elementary Student
This example addresses emotional regulation interventions for a young client:
S: "A 10-year-old client reports feeling ‘worried all the time’ and experiencing difficulty sleeping. The mother notes increased irritability, frequent stomachaches, and avoidance of school-related tasks over the past month."
O: "During the session, the student appeared anxious, exhibiting fidgeting behaviors and difficulty maintaining eye contact. The student demonstrated shallow breathing patterns and a tense posture. The session included a 20-minute practice of deep breathing techniques and progressive muscle relaxation, with the student following verbal cues successfully."
A: "The student presents with anxiety symptoms that affect school performance and daily functioning. However, the student shows good potential for learning coping strategies and is willing to practice the techniques, bolstered by strong family support for home practice."
P: "Continue teaching relaxation techniques, including deep breathing and progressive muscle relaxation. Assign daily practice homework for home implementation and schedule a follow-up in one week to assess progress and adjust intervention strategies as needed."
Good vs. Poor SOAP Note Entries
The quality of documentation can significantly impact patient outcomes. Research shows that structured documentation templates improve note quality by 36.6% while reducing documentation time by 42%.
| Aspect | Effective SOAP Note | Ineffective SOAP Note |
|---|---|---|
| Language | Clear, concise, and detailed | Vague, incomplete, or disorganized |
AI Tools for OT Documentation
With the increasing demand for accurate and detailed SOAP notes, AI tools are stepping in to simplify and improve the documentation process. For occupational therapists (OTs), these tools not only reduce administrative burdens but also enhance the precision and efficiency of their documentation.
DocScrib Features for OTs
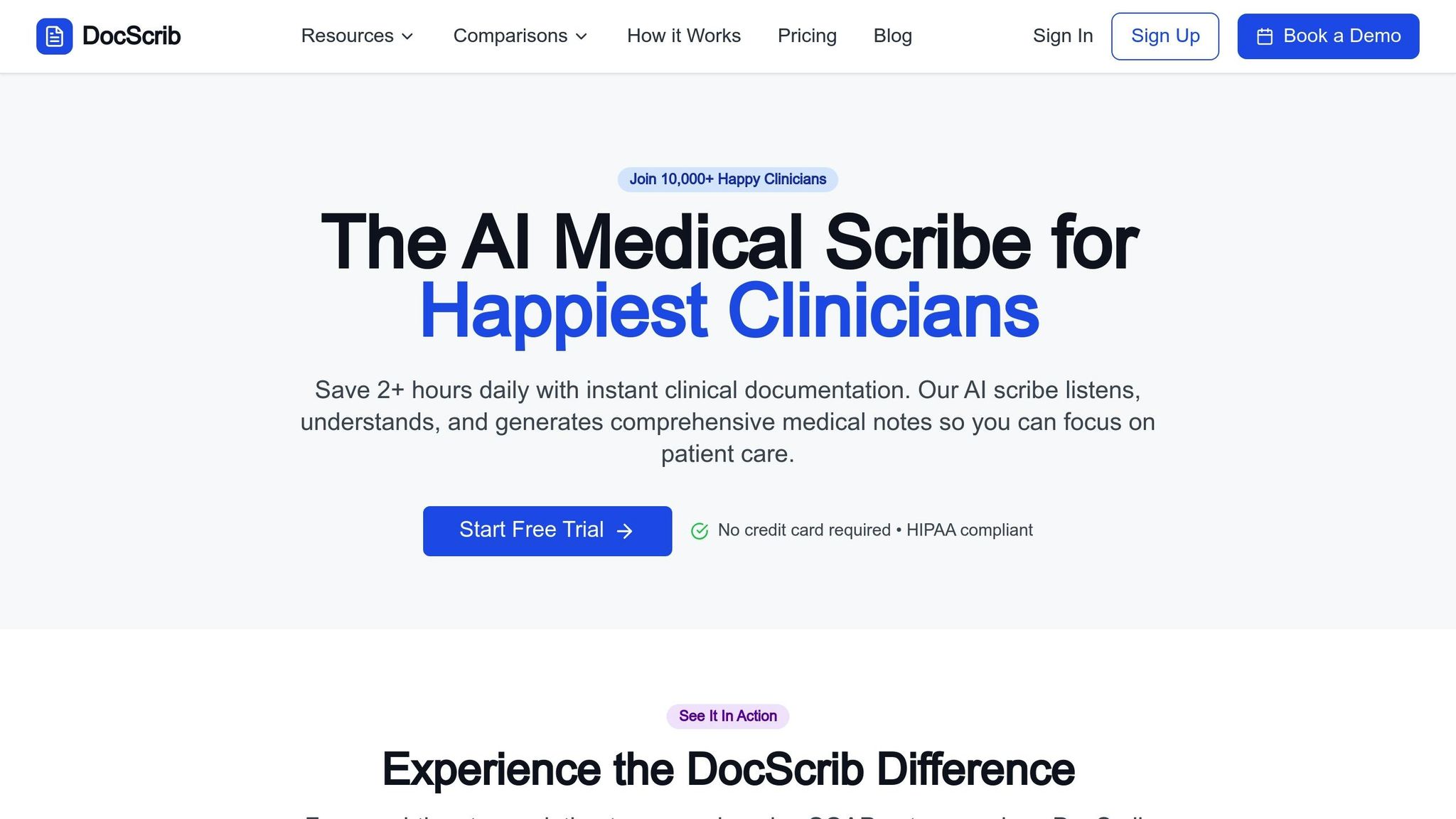
DocScrib is designed to tackle the specific challenges OTs face when documenting their work, offering a streamlined process from session notes to final reports.
- Real-time transcription: This feature captures spoken words during therapy sessions, allowing therapists to focus entirely on their patients without worrying about taking notes. By automating the documentation, OTs can engage in more natural and uninterrupted conversations with clients, improving the therapeutic experience.
- Customizable templates: Built to align with occupational therapy workflows, these templates follow the SOAP note structure but can be adjusted to fit specific assessment tools and intervention strategies. Whether you’re working in pediatric care or adult rehabilitation, the templates can adapt to meet your practice’s needs.
- HIPAA compliance: Security is a top priority. DocScrib ensures patient data is protected with encryption, secure storage, and strict access controls, meeting all federal healthcare privacy standards.
- EHR integrations: The platform connects seamlessly with electronic health record systems, eliminating redundant data entry and centralizing patient information. This integration not only reduces errors but also ensures that patient records are easily accessible across providers.
These features directly address the challenges OTs encounter, paving the way for more efficient workflows and better patient care.
How AI Tools Solve Documentation Problems
AI tools are transforming the way clinicians handle documentation, allowing them to dedicate their full attention to patients. In fact, clinics using AI tools report a 67% increase in patient session attendance, highlighting their impact on both efficiency and outcomes.
One key advantage is the reduction of task-switching. Therapists no longer need to pause sessions to jot down notes or rely on memory to recall details later. This uninterrupted flow fosters more natural interactions and enables therapists to better assess patient responses in real time.
Additionally, AI tools help standardize compliance practices. They can be tailored to match a therapist’s documentation style while ensuring that all required details are consistently recorded. This minimizes the risk of missing critical information or failing to meet regulatory standards.
Error reduction is another major benefit. Unlike traditional copy-and-paste methods, which can lead to inconsistencies, AI-powered transcription and EHR integration provide real-time, automated documentation. This approach significantly lowers the chances of forgetting observations or misremembering patient details.
With these advantages in mind, choosing the right AI solution is essential for optimizing practice workflows.
DocScrib Pricing Plans
DocScrib offers three pricing options tailored to different practice sizes and documentation needs. Each plan includes essential AI features, with additional tools for more advanced requirements.
| Plan | Monthly Price | Patient Visits | Key Features | Best For |
|---|---|---|---|---|
| Starter | $49 | Up to 100 | Real-time transcription, basic templates, HIPAA-compliant storage, email support | Individual practitioners, new practices |
| Professional | $99 | Up to 500 | Advanced AI note generation, custom templates, priority support, analytics dashboard, up to 3 users | Busy practitioners, small clinics |
| Enterprise | Custom pricing | Unlimited | Robust security, custom AI training, dedicated account manager, 24/7 support, unlimited users | Large practices, health systems |
- The Starter plan is ideal for solo practitioners or new practices, offering essential features like real-time transcription and basic SOAP note templates for just $49 per month.
- The Professional plan, priced at $99 per month, is geared toward busier practices with up to 500 patient visits. It includes advanced note generation, an extensive template library, and an analytics dashboard, supporting up to three users – perfect for small clinics.
- The Enterprise plan is customized for large practices or health systems. It provides unlimited patient visits, custom AI model training, and dedicated 24/7 support, making it suitable for organizations with extensive documentation needs.
When evaluating AI documentation tools, ensure they are HIPAA-compliant and inquire about their real-world impact on documentation efficiency. This will help confirm that the tool delivers measurable improvements in both time savings and workflow optimization.
sbb-itb-5a50404
OT SOAP Notes Cheat Sheets
Creating efficient and accurate SOAP notes becomes much simpler with quick-reference tools. These cheat sheets put essential information at your fingertips, so you can focus on documentation without constantly searching for abbreviations, conversions, or assessment details.
Common OT Documentation Abbreviations
Abbreviations are a cornerstone of efficient OT documentation. They save time but must be used with caution to avoid miscommunication. Stick to approved abbreviations within your electronic medical records (EMR) system to ensure clarity and consistency. Many EMRs now include text expander features, which automatically convert abbreviations into full phrases – helping you work faster while reducing errors.
| Category | Abbreviation | Meaning |
|---|---|---|
| Functional Status | ADL | Activities of Daily Living |
| IADL | Instrumental Activities of Daily Living | |
| I/Indep | Independent | |
| Max A | Maximum Assistance | |
| Mod A | Moderate Assistance | |
| Min A | Minimum Assistance | |
| SBA | Standby Assist | |
| CGA | Contact Guard Assistance | |
| Movement & Range | AROM | Active Range of Motion |
| PROM | Passive Range of Motion | |
| AAROM | Active Assistive Range of Motion | |
| UE | Upper Extremity | |
| LE | Lower Extremity | |
| RUE | Right Upper Extremity | |
| LUE | Left Upper Extremity | |
| Weight Bearing | FWB | Full Weight Bearing |
| PWB | Partial Weight Bearing | |
| WBAT | Weight Bearing As Tolerated | |
| NWB | Non-Weight Bearing | |
| TTWB | Toe Touch Weight Bearing | |
| Equipment & Devices | DME | Durable Medical Equipment |
| AD | Assistive Device | |
| W/C | Wheelchair | |
| AFO | Ankle Foot Orthosis | |
| KAFO | Knee Ankle Foot Orthosis | |
| SPC | Single Point Cane | |
| Medical Conditions | TBI | Traumatic Brain Injury |
| CVA | Cerebrovascular Accident | |
| SCI | Spinal Cord Injury | |
| TKA | Total Knee Arthroplasty | |
| THR | Total Hip Replacement | |
| OA | Osteoarthritis | |
| Assessment Terms | WFL | Within Functional Limits |
| WNL | Within Normal Limits | |
| MMT | Manual Muscle Test | |
| ROM | Range of Motion | |
| BOS | Base of Support |
Pro tip: Use EMR shortcuts to integrate these abbreviations into your notes and speed up your workflow.
Measurement Conversions and Standards
Accurate measurements are just as important as abbreviations in OT documentation. Whether you’re recording equipment specs, range of motion, or spatial assessments, proper conversions ensure reliable patient records.
Length Conversions:
- 1 inch = 2.54 centimeters = 25.4 millimeters
- 1 foot = 30.48 centimeters = 0.3048 meters
- 1 yard = 0.91 meters
- 1 mile = 1.61 kilometers
Common OT Measurement Applications:
- Goniometer readings: Recorded in degrees (°).
- Grip strength: Measured in pounds (lbs) or kilograms (kg).
- Wheelchair measurements: Width in inches; weight capacity in pounds.
- Transfer distances: Measured in feet or meters.
In the U.S., healthcare documentation typically uses imperial measurements, despite the legal adoption of the metric system as early as 1866. Conversion skills are essential for accuracy in records.
"The metric system has been legal in this country since 1866." – Don Hillger, president of the U.S. Metric Association
Common OT Assessment Tools
Choosing the right assessment tool is key to documenting patient progress effectively. While the American Occupational Therapy Association (AOTA) does not endorse specific tools, practitioners should rely on clinical judgment to select the best options for each case.
| Assessment | Population | Time Required | Primary Use |
|---|---|---|---|
| Canadian Occupational Performance Measure (COPM) | All ages with activity limitations | 30–60 minutes | Evaluates performance and satisfaction with daily activities |
| Assessment of Motor and Process Skills (AMPS) | All ages with functional difficulties | 1–2 hours | Observation-based task performance |
| Modified Barthel Index (MBI) | Adults with physical disabilities | 10–15 minutes | Assesses basic ADL independence |
| Functional Independence Measure (FIM) | Adults in rehabilitation | 60–90 minutes | Provides a comprehensive functional assessment |
| Mini-Mental State Examination (MMSE) | Adults with cognitive concerns | 5–10 minutes | Cognitive screening |
| Pediatric Evaluation of Disability Inventory (PEDI) | Children birth to 7 years | 60–90 minutes | Evaluates functional abilities in children |
| Sensory Profile | Children and adults | 30–45 minutes | Assesses sensory processing patterns |
| Peabody Developmental Motor Scales (PDMS) | Infants to preschoolers | 45–60 minutes | Measures gross and fine motor development |
| School Function Assessment (SFA) | School-aged children | 60–90 minutes | Assesses school-based functional performance |
| Timed Up and Go (TUG) | Older adults | 5–10 minutes | Measures mobility and fall risk |
| Functional Reach Test | Adults and older adults | 5–10 minutes | Evaluates balance and predicts fall risk |
Documentation Tips: When recording assessment results, always include the tool used, raw scores (or percentiles/standard scores, if relevant), and your professional interpretation. This ensures clarity for other team members and consistency in future evaluations.
Assessments should address relevant occupations, client factors, performance skills, and the client’s environment. Choose tools that best capture the abilities and needs of your client, and document results in a way that’s clear and easy to replicate.
OT Documentation Best Practices and Common Mistakes
When it comes to Occupational Therapy (OT) documentation, precision and clarity can make all the difference. Building on solid SOAP note examples and leveraging AI tools, you can take your documentation to the next level by following proven best practices while steering clear of common errors. Proper documentation isn’t just about compliance – it’s about improving clinical outcomes and ensuring accurate communication.
Tips for Writing Better SOAP Notes
Write notes immediately after sessions. Research shows that delays in documentation can lead to memory gaps and inaccuracies. Aim to complete your notes within 10–15 minutes after each session to capture precise details while they’re still fresh.
Be specific and measurable. Avoid vague language like "patient is improving." Instead, provide concrete data: "Grip strength increased from 15 lbs to 22 lbs over two weeks" or "Patient completed dressing tasks with moderate assistance (50% physical prompting) compared to maximum assistance (75%) during the initial evaluation." This level of detail supports clinical decisions and insurance requirements.
Connect impairments to daily life. Show how specific impairments impact functional activities. For instance, "Decreased shoulder flexion (85° active ROM) limits the patient’s ability to reach items on standard kitchen shelves, requiring a reacher or reorganization of frequently used items."
Set SMART goals. Always outline goals that are specific, measurable, achievable, relevant, and time-bound. For example: "Patient will independently don a pullover shirt within 5 minutes using adaptive techniques within 3 weeks."
Highlight strengths and progress. Frame progress in a positive light without ignoring limitations. Instead of writing "patient failed to complete task", try "patient completed 3 of 5 steps independently, requiring verbal cues for the final two steps."
Use technology wisely. Tools like voice-to-text can cut documentation time significantly, and electronic health record templates can provide consistency. However, always tailor each note to reflect the specifics of the session.
Streamline your workflow. Create a system for efficient documentation. For example, prioritize urgent tasks using tools like the Eisenhower Matrix, jot down brief session notes during treatment, and allocate specific time blocks for writing detailed notes later.
Common Documentation Errors to Avoid
Even the best practices can be undermined by a few common missteps. Here are some frequent mistakes to watch out for:
Mixing up SOAP sections. Each section has a purpose. The Objective section should contain measurable, observable data, while the Assessment section is for clinical judgments. For instance, "patient appeared frustrated" belongs in the Assessment, while "patient required 3 verbal prompts to complete the task" fits in the Objective.
Overusing copy-paste. Reusing old text can lead to inaccuracies and compliance risks. Each note must reflect the unique details of the session. Auditors often flag repetitive language patterns as a sign of poor documentation practices.
Delaying documentation. Waiting days or weeks to write notes increases the risk of memory errors and creates liability issues. Timely documentation is crucial for accuracy and compliance, as delayed entries can raise red flags with Medicare and insurance auditors.
Using unclear abbreviations. Stick to standard medical abbreviations or those approved by your facility’s EMR system. Avoid clinic-specific jargon that could confuse other providers. When in doubt, spell it out.
Failing to link interventions to goals. Every intervention should tie back to a specific treatment goal. If an activity doesn’t clearly advance a measurable goal, reconsider its inclusion in the plan. This connection is vital for reimbursement and audit compliance.
Writing vague or passive notes. Phrases like "tolerated well", "seemed to enjoy", or "appeared to understand" lack precision. Instead, use specific observations: "Completed a 15-minute activity without rest breaks" is far more effective than "tolerated activity well".
Ignoring compliance standards. Missing required elements – like justification for skilled intervention or evidence of medical necessity – can lead to claim denials or penalties. Stay updated on Medicare and payer-specific guidelines to ensure your documentation meets all requirements.
Making general statements about progress. Avoid blanket phrases like "patient shows good progress" without supporting evidence. Be specific: document exactly what improvements occurred, how much progress was made, and over what time period.
Conclusion
SOAP notes, when done right, can completely transform the way occupational therapists manage their workflows. By blending structured documentation with modern tools, therapists can improve both efficiency and the quality of care they provide. These changes don’t just streamline processes – they also bring measurable clinical and financial benefits.
AI tools take this transformation to the next level. For example, DocScrib has changed the game for occupational therapists. Clinicians using this tool have reported saving a significant amount of time, with documentation taking up to 70% less time. Even more impressively, therapists experienced a 30–40% reduction in self-reported burnout after just six weeks of use.
The cheat sheets and best practices shared in this guide are designed to help therapists maximize these benefits. When paired with AI tools, therapists who refine their documentation skills report spending 30% less time on paperwork. That means more hours available for what truly matters: direct patient care. It’s about working smarter while maintaining the high standards that occupational therapy demands.
Mastering documentation is a skill that improves with time and the right resources. Whether it’s leveraging AI-powered features from DocScrib, using standardized cheat sheets, or sticking to proven methods, each step contributes to a system that works for both therapists and patients. This integrated approach ensures that workflows not only run smoothly but also support better patient outcomes.
Today, occupational therapy documentation is all about prioritizing patient care by improving accuracy and efficiency. With detailed, well-structured records, therapists can support the best possible outcomes for their patients.
FAQs
How does DocScrib help occupational therapists save time when writing SOAP notes?
DocScrib is transforming the way occupational therapists handle documentation by leveraging AI-powered tools to create SOAP notes effortlessly. It listens to patient interactions and organizes clinical information into structured notes in real-time, ensuring precision while cutting down documentation time.
By simplifying the documentation process, DocScrib frees up therapists to dedicate more time to their patients instead of administrative duties. This shift not only enhances workflow efficiency but also helps alleviate burnout, all while maintaining compliance with healthcare documentation standards.
What are some key mistakes to avoid when writing SOAP notes in occupational therapy?
When writing SOAP notes in occupational therapy, steering clear of common errors is essential for maintaining both clarity and precision. Here are some key missteps to watch out for:
- Omitting important details: Forgetting to include things like vital signs, specific test results, or measurable outcomes can leave the note incomplete and less useful.
- Using vague or unsupported language: General statements without evidence can weaken the clinical reasoning behind your notes.
- Delaying documentation: Writing notes too long after a session can lead to forgotten details and potential inaccuracies.
- Overloading with jargon: Excessive use of professional terms without explanations can confuse other healthcare professionals or readers.
- Repetition: Repeating information unnecessarily can clutter your notes and make them harder to follow.
By being aware of these pitfalls, you can ensure your SOAP notes are clear, concise, and effective, ultimately improving both your documentation process and patient care.
How does each section of a SOAP note improve patient care and ensure accurate documentation?
Each part of a SOAP note serves an important purpose in ensuring effective patient care and precise documentation. The Subjective section captures the patient’s own words – detailing their symptoms, concerns, and experiences. This personal insight allows healthcare providers to address the patient’s unique needs. The Objective section focuses on measurable clinical information, such as lab results, physical exam findings, or observable signs, providing a factual foundation for the note. The Assessment combines these subjective and objective pieces, offering a clear narrative of the patient’s condition, progress, or challenges. Lastly, the Plan lays out the next steps in treatment, detailing actionable strategies to maintain continuity and accountability in care.
When properly utilized, SOAP notes not only improve communication among healthcare professionals but also streamline daily workflows and support compliance with legal and regulatory standards. This structured format ensures thorough and efficient documentation, benefiting both patients and providers alike.