Updated on: July 30, 2025
Mediastinal lymphadenopathy—the abnormal enlargement of lymph nodes within the central chest cavity—can signal anything from benign infections to metastatic malignancies. For clinicians, especially those in pulmonary, oncology, and internal medicine, accurately identifying, documenting, and coding this condition is essential for delivering timely and targeted care.
This article will explore:
-
What mediastinal lymphadenopathy is and what causes it
-
How to identify and differentiate serious underlying conditions
-
Best practices for ICD-10 coding (including R59.1)
-
Common documentation gaps and how to fix them
-
How DocScrib transforms how you chart and bill for complex cases
What Is Mediastinal Lymphadenopathy?
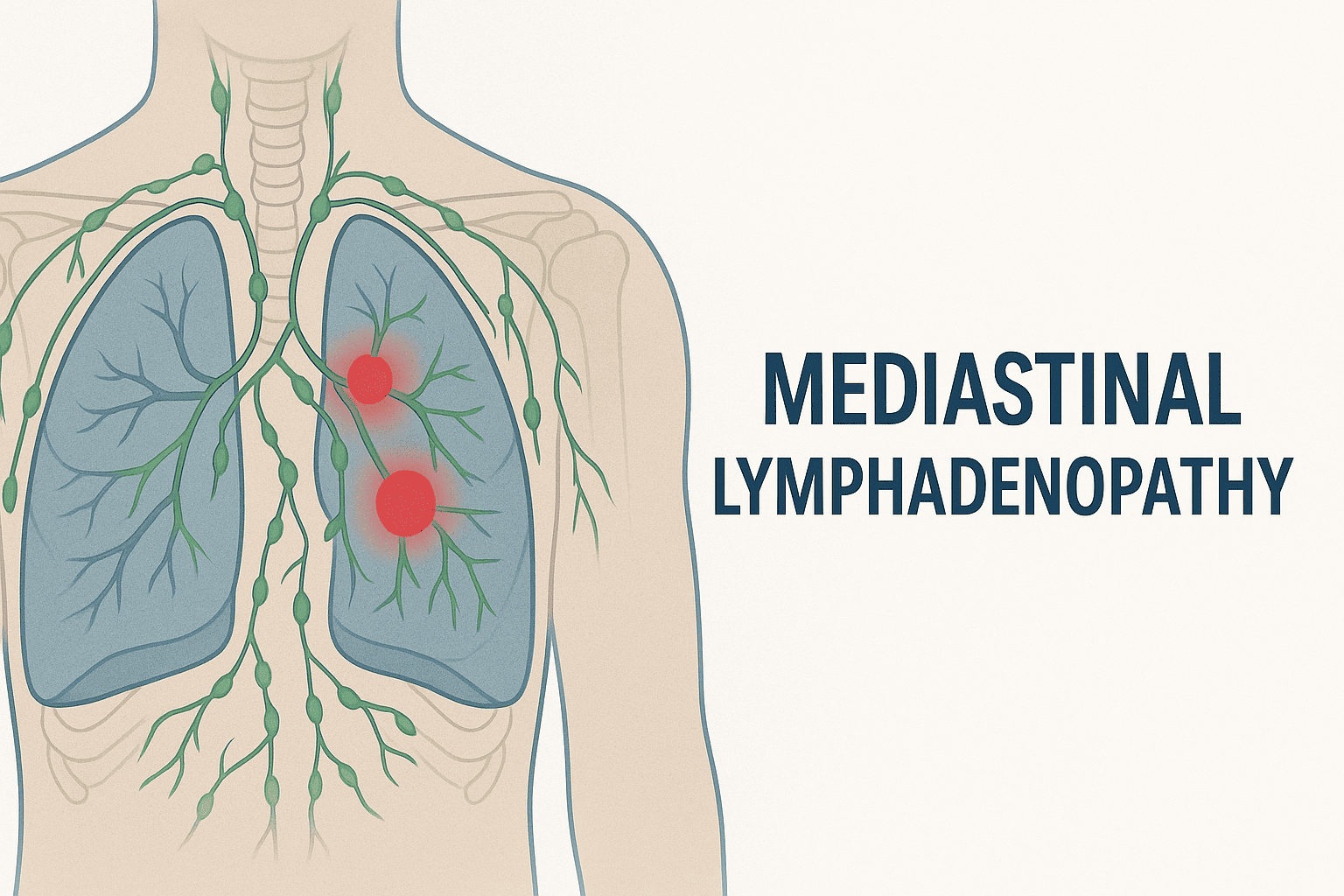
Mediastinal lymphadenopathy refers to enlarged lymph nodes located in the mediastinum, the central compartment of the thoracic cavity that contains the heart, trachea, esophagus, and associated lymphatic tissue.
Lymph nodes are considered abnormal if they exceed:
-
>10 mm in short-axis diameter on CT scan, or
-
>15 mm for certain hilar nodes, depending on radiologic criteria
Mediastinal lymphadenopathy may be incidental, inflammatory, or a hallmark of serious pathology such as lymphoma, sarcoidosis, or metastatic cancer.
Common Causes of Mediastinal Lymphadenopathy
| Etiology | Examples |
|---|---|
| Infectious | Tuberculosis, Histoplasmosis, COVID-19, HIV |
| Neoplastic | Lung cancer, lymphoma, metastatic breast or GI tumors |
| Autoimmune | Sarcoidosis, rheumatoid arthritis, SLE |
| Environmental | Pneumoconiosis, berylliosis |
| Idiopathic | In some asymptomatic cases after viral infections |
📌 Always correlate imaging with clinical presentation and laboratory data to avoid misdiagnosis.
Symptoms That May Accompany Mediastinal Lymphadenopathy
-
Cough (dry or productive)
-
Chest discomfort or pain
-
Shortness of breath
-
Fever or night sweats
-
Weight loss (in malignancies)
-
Hemoptysis (in advanced TB or cancer)
In many cases, the lymphadenopathy is incidentally discovered during evaluation for unrelated conditions, especially on chest CTs or PET scans.
ICD-10 Coding for Mediastinal Lymphadenopathy
Accurate coding ensures proper reimbursement, risk adjustment, and follow-up tracking. The choice of ICD-10 code depends on the underlying cause and whether a definitive diagnosis has been established.
Common ICD-10 Codes:
| ICD-10 Code | Description | Use When… |
|---|---|---|
| R59.1 | Enlarged lymph nodes, intrathoracic | Lymphadenopathy is noted but cause is still under evaluation |
| I89.1 | Lymphangitis | Inflammation of lymphatic vessels present |
| C77.1 | Secondary and unspecified malignant neoplasm of intrathoracic lymph nodes | Lymphadenopathy due to metastatic disease (e.g., lung cancer) |
| D47.Z9 | Neoplasm of uncertain behavior of lymphoid tissue | When lymphoma is suspected but not confirmed |
| A15.0 | Tuberculosis of lung with confirmed diagnosis | If TB is established as the cause |
| D86.0 | Sarcoidosis of lung | For sarcoidosis with hilar/mediastinal node involvement |
✅ Use R59.1 as a placeholder or symptom code until a definitive diagnosis is confirmed.
Sample Documentation for Mediastinal Lymphadenopathy
Subjective:
“Patient reports persistent dry cough for the last three weeks. No weight loss or hemoptysis. No known TB exposure. No prior cancer history.”
Objective:
CT chest: enlarged subcarinal and paratracheal lymph nodes measuring 14 mm. No obvious parenchymal mass. No pleural effusion.
Assessment:
Mediastinal lymphadenopathy under investigation. Likely differential includes infectious (e.g., TB), inflammatory (sarcoidosis), or neoplastic.
Plan:
-
Order TB Quantiferon Gold and ACE levels
-
Refer to pulmonology for bronchoscopy
-
ICD-10 Code: R59.1 – Intrathoracic lymphadenopathy
Key Elements to Document
✔️ Size and location of lymph nodes (subcarinal, paratracheal, hilar)
✔️ Symptoms or lack thereof
✔️ Imaging findings and any associated lesions
✔️ Planned workup (labs, biopsy, bronchoscopy, PET scan)
✔️ Suspicion for cancer vs. infection vs. autoimmune
Common Documentation Pitfalls
🚫 Vague language like “abnormal CT” or “rule out malignancy”
🚫 Missing anatomical specificity (e.g., mediastinal vs. cervical)
🚫 Lack of correlation with symptoms or diagnostic plans
🚫 Not updating code when diagnosis becomes definitive (e.g., switching from R59.1 to C77.1)
How DocScrib Simplifies Charting Mediastinal Lymphadenopathy
Manually documenting radiology findings, ICD-10 codes, and diagnostic plans for conditions like mediastinal lymphadenopathy can be time-consuming—especially in high-volume specialties like pulmonology, oncology, and critical care.
DocScrib solves this problem by:
✅ Auto-extracting anatomical terms like “mediastinal,” “subcarinal,” or “hilar nodes”
✅ Suggesting the correct ICD-10 code (e.g., R59.1, C77.1, D86.0)
✅ Generating pre-structured SOAP or H&P notes
✅ Capturing radiology interpretations and follow-up plans in real time
✅ Reducing documentation time by up to 70%
Streamline oncology and pulmonary charting today
👉 Book your free DocScrib demo
Quick Reference Table: Mediastinal Lymphadenopathy Coding by Scenario
| Clinical Situation | ICD-10 Code(s) |
|---|---|
| Unexplained mediastinal lymphadenopathy | R59.1 |
| Known lung cancer with nodal spread | C34.x + C77.1 |
| Suspected lymphoma pending biopsy | D47.Z9 + R59.1 |
| Sarcoidosis with node enlargement | D86.0 |
| TB confirmed by labs/biopsy | A15.0 or A16.0 |
| Post-COVID reactive lymphadenopathy | U09.9 + R59.1 |
FAQs
Q1: Should I use R59.1 even if the lymphadenopathy is incidental?
Yes. If it’s clinically documented and being monitored or evaluated, R59.1 is appropriate—even if asymptomatic.
Q2: What if the underlying cause becomes known later (e.g., cancer)?
Update the diagnosis and ICD-10 code (e.g., switch to C77.1 if metastasis is confirmed). This ensures accurate reporting and billing.
Q3: Can I code both R59.1 and the final diagnosis?
Yes, especially during initial evaluation and ongoing diagnostic workup.
Q4: Does DocScrib integrate radiology findings into SOAP notes?
Yes. DocScrib pulls relevant radiologic phrases into structured notes and prompts appropriate coding.
Q5: How often should I follow up on incidental mediastinal lymphadenopathy?
Depends on size, growth rate, and patient risk factors. Many require 3- to 6-month imaging surveillance.
Final Thoughts
Mediastinal lymphadenopathy may be incidental, inflammatory, or a red flag for systemic disease. Whether you’re monitoring a suspicious node or staging a malignancy, clear documentation and proper ICD-10 coding—starting with R59.1—are vital.
With AI-powered tools like DocScrib, clinicians can transform radiology findings into structured, audit-proof documentation—all while saving time and improving patient care.
👉 Book your free demo today and see how DocScrib makes pulmonary and oncology charting smarter and faster.