Updated on: July 2, 2025
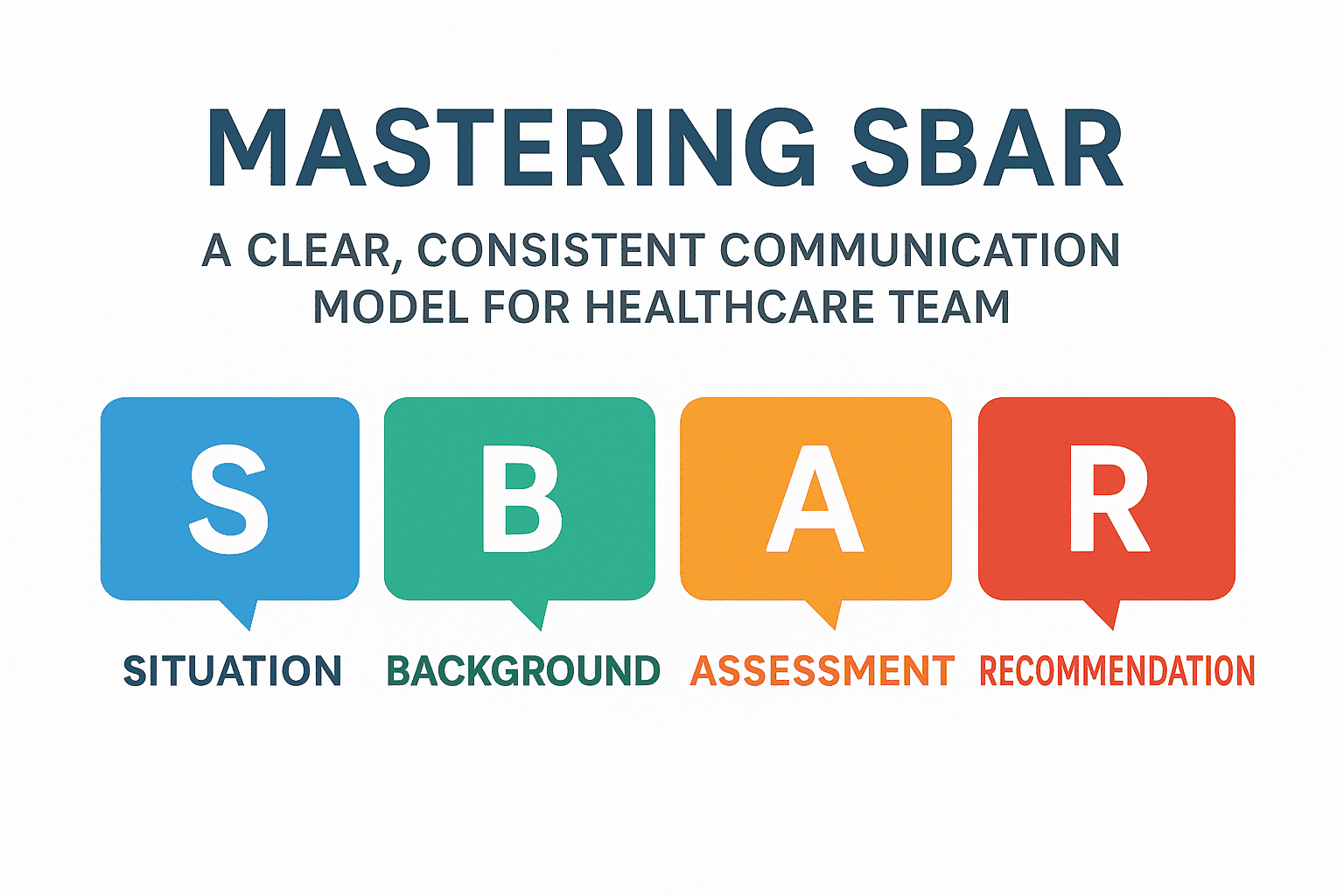
Effective communication in healthcare saves lives—and the SBAR (Situation‑Background‑Assessment‑Recommendation) framework is one of the most proven tools to ensure clarity in urgent or routine handoffs.
1. What Is SBAR and Why It Matters
SBAR stands for Situation, Background, Assessment, Recommendation.
Originated in the U.S. Navy in the 1940s, later adopted across aviation and nuclear subs before entering healthcare, with wide implementation at Kaiser Permanente and endorsement by bodies like the Royal College and IHI
asq.org.
According to the Joint Commission, about 80% of serious medical errors stem from miscommunication—SBAR offers structure to reduce those mistakes
heidihealth.com
2. SBAR Breakdown: What Goes Into Each Section
Situation
One-sentence overview: patient identity, immediate issue, and urgency.
Example:
“Dr. Patel, this is Nurse Lee from CCU. Mr. Ramirez in Room 12 has developed sudden-onset chest pain radiating to his arm and jaw—BP is 145/95 and HR is 110.”
Background
Vital context: current diagnosis, relevant history, recent labs/vitals.
Example:
“He was admitted 24 hrs ago with NSTEMI, started on aspirin, heparin, and beta-blocker; no known drug allergies.”
Assessment
Your clinical view and interpretation—what YOU think.
Example:
“Given escalating chest discomfort, rising troponins, and persistent tachycardia, I’m concerned about ongoing ischemia or evolving MI.”
Recommendation
Specific request or next steps for the team.
Example:
“Please order an urgent cardiology consult, repeat ECG, and chest pain panel. Should I prepare for transfer to CCU?”
3. Proven Benefits of SBAR
Consistency: ensures no vital info is omitted during handoffs
mhanet.com
Clarity: organizes the thought process, preventing rambling or assumptions .
Empowerment: nurses and allied staff confidently present clinical concerns—even in high-stress moments
youtube.com.
4. Real SBAR Example in Practice
Situation: “Dr. Singh, this is Nurse Patel in Ward 5. Ms. Thomas, a 68‑year‑old admitted for hip surgery, now has a BP of 80/50, HR 130, and is reporting dizziness.”
Background: “She’s 48 hours post-op, on IV fluids, no bleeding at incision, hemoglobin dropped from 11 to 8.5 g/dL.”
Assessment: “I suspect postoperative anemia or possible internal bleeding—seems hemodynamically unstable.”
Recommendation: “Recommend CBC stat, IV fluid bolus, check coagulation, and call surgery resident for evaluation.”
5. Best Practices & Common Pitfalls
Best Practices Common Pitfalls
Use pre-call prep: review charts, labs, vitals Overloading with unnecessary data
Lead with most urgent info—Situation first Vague or missing recommendations
Be precise in Assessment (“I think…”), not diagnosing Not clarifying the action or timing needed
Confirm next steps (“Will you…?”) Failure to document the exchange
6. Customizing SBAR for Your Setting
Psychiatry: add mental status updates or risk notes.
ICU/Emergency: include ventilator settings or relevant bedside data.
Telemedicine: emphasize vital timelines (“10 mins ago BP dropped”) and clarity.
Modify SBAR to include extra fields like Current Meds, Allergies, or Recent Imaging as needed.
7. Taking SBAR to the Next Level with Tech
Digital tools can auto-populate structured SBAR reports:
DocScrib’s platform can use built-in templates for SBAR with real-time data pull, making handoffs faster and more accurate.
AI-powered scribes like Heidi can transcribe and organize dialogue in SBAR format, minimizing omissions
mhanet.com.
8. How to Implement SBAR at Your Facility
Train staff with role-play and scenario drills.
Use visual aids: posters, pocket cards, or EHR templates.
Audit usage: spot-check communications and note documentation.
Iterate: encourage feedback—adapt sections for specialty, setting, or user role.
In Summary
SBAR is a concise communication tool proven to reduce errors and improve teamwork.
Structure it into Situation ➝ Background ➝ Assessment ➝ Recommendation.
Customize it for your environment, and enhance accuracy with digital tools.
Practice and audit use—successful handoffs depend just as much on adoption as structure.
🧩 Try This: SBAR Template
markdown
Copy
Edit
**S: Situation**
• [Your Name], [Unit]. Patient [Name], [Age], [Room]: [Presenting Problem]
**B: Background**
• Admitted for [Diagnosis], on [Meds], allergies: [List]
• Relevant labs/vitals: [e.g., Hb, BP, HR]
**A: Assessment**
• [Your impression]
**R: Recommendation**
• I recommend [Action]—[Who], [When]
Embed this in DocScrib as a fillable template for consistent documentation and communication.
By integrating SBAR into routine practice—and enhancing with digital precision—you’ll help your team communicate more effectively, reduce preventable errors, and improve patient care. Let me know if you’d like image templates, downloadable assets, or success stories tailored to DocScrib’s users!