Updated on: July 24, 2025
Introduction
In today’s clinical practice, precise documentation is more than just a formality—it’s a gateway to timely reimbursement, fewer claim denials, and better patient record management. At the heart of this process are CPT® codes—five-digit identifiers used to describe the procedures and services provided by healthcare professionals. This comprehensive guide helps clinicians, billers, and practice administrators understand where and how to look up CPT® codes accurately and efficiently.
What Are CPT® Codes?
Current Procedural Terminology (CPT®) codes were created by the American Medical Association (AMA) to standardize the way medical services are reported and billed. They serve as the universal language for reporting healthcare procedures to payers, government agencies, and data registries.
Categories of CPT® Codes:
- Category I – Widely used medical services and procedures (e.g., office visits, lab tests).
- Category II – Supplemental performance measurement tracking codes.
- Category III – Temporary codes for emerging or experimental procedures.
CPT® vs. ICD-10 vs. HCPCS:
- CPT® = Procedures
- ICD-10 = Diagnoses
- HCPCS = Supplies and services not in CPT®
CPT® codes are updated annually and are proprietary to the AMA. Accessing the most accurate and updated versions typically requires AMA-licensed tools or partnerships.
Why and When to Look Up CPT® Codes
There are several scenarios in which a clinician or billing team may need to look up a CPT® code:
- You’re performing a new procedure or delivering a telehealth service and need an accurate code.
- Insurance policies change, requiring code updates or new documentation rules.
- You’re validating whether a modifier (e.g., -25 or -59) applies to your claim.
- You’re conducting internal audits to reduce upcoding or unbundling.
- You want to verify reimbursement rates or coverage.
Getting it wrong can lead to claim denials, audits, or underpayment.
Top Methods to Locate the Right CPT® Code
AMA CPT® Search Tool
The AMA offers an official online search engine for CPT® codes. Although it provides limited free searches daily, it’s one of the most accurate resources. It includes code descriptions, references, and category tags.
EHR or Practice Management Software
Many electronic health record systems and practice management tools have built-in CPT® lookup tools. These are integrated into workflows so providers can assign codes during documentation.
Subscription-Based Tools (Codify, AAPC, Find‑A‑Code)
- Codify by AAPC provides advanced lookup with NCCI edits, crosswalks, and payer-specific requirements.
- Find‑A‑Code allows simultaneous CPT®, ICD-10, and HCPCS lookups with bundled resources and intuitive design.
These tools are ideal for billing professionals who need speed and accuracy in claim submission.
Free Specialty-Specific Guides
Organizations often publish free guides with relevant CPT® codes for therapists, occupational therapists, speech-language pathologists, etc. These include details about evaluation codes, therapy codes, and modifiers.
Step-by-Step Guide: How to Look Up a CPT® Code
Here’s a general process that clinicians and billers can follow:
- Identify the Service or Procedure: Is it an evaluation? A therapy session? A surgical procedure?
- Use a Reliable Source: Choose from AMA search, EHR-integrated lookup, or coding software.
- Refine by Context: Consider patient age, time duration, provider type, and modifiers.
- Check for Updates: Confirm that the code is current and active.
- Validate Against ICD-10/HCPCS: Ensure alignment with diagnosis and supplies used.
- Apply NCCI Edits: Check for bundling/unbundling rules and modifier allowances.
This flow reduces coding errors and billing rejections.
Most Common CPT® Codes in Behavioral Health
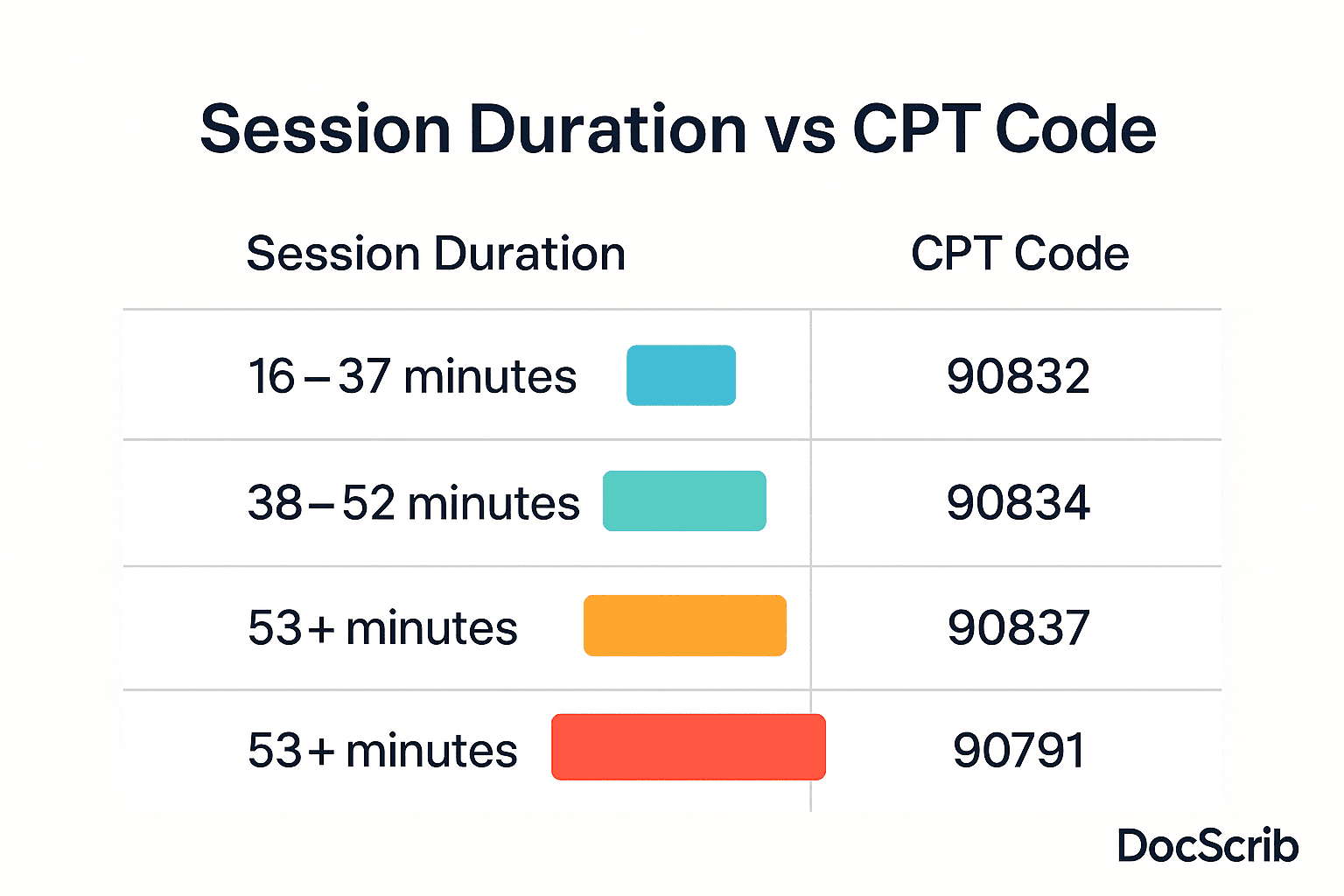
| Code | Description | Session Duration |
|---|---|---|
| 90791 | Psychiatric diagnostic evaluation | Initial assessment |
| 90832 | Psychotherapy | 16–37 minutes |
| 90834 | Psychotherapy | 38–52 minutes |
| 90837 | Psychotherapy | 53+ minutes |
| 90785 | Interactive complexity add-on | Add-on to therapy |
| 90839 | Crisis psychotherapy (first 60) | Initial 60 mins |
| 90840 | Crisis psychotherapy (each add’l) | Add-on to 90839 |
Therapists must document session times accurately and note any complexity or crisis involvement for proper billing.
CPT® Reimbursement Trends
Data suggests that reimbursement rates for the same CPT® code can vary depending on geography, payer type, and specialty. For example:
- 90837 (53+ min therapy) may be reimbursed at:
- $90–$140 in most states
- Higher in urban areas or private payers
This variance means coding and payer negotiation should go hand-in-hand. Clinicians should regularly review their top CPT® codes for rate updates and modifiers affecting payment.
Common Pitfalls and Errors
- Upcoding: Billing for a higher-level service than provided.
- Unbundling: Billing separately for services that are covered under a single comprehensive code.
- Using outdated codes: CPT® codes change annually; using old codes may trigger denials.
- Missing modifiers: Some procedures require add-on modifiers (e.g., -95 for telehealth).
- Poor documentation: Lack of session time or treatment detail can invalidate the CPT® used.
Avoiding these errors ensures better compliance and improved cash flow.
CPT® and Medicare/HCPCS Considerations
- CPT® forms the backbone of Medicare billing, but some services may require HCPCS Level II codes.
- Medicare also enforces National Correct Coding Initiative (NCCI) rules to prevent improper billing.
- Billing Medicare? Ensure you check Medicare Physician Fee Schedule (MPFS) for rates and coverage.
Staying Updated with CPT® Code Changes
- Annual Updates: Every October, the AMA publishes the CPT® code set for the following year.
- Monthly Bulletins: EHRs and coding software often include monthly change alerts.
- Professional Associations: Many send newsletters or provide webinars on CPT® code changes.
- Audit Alerts: Stay aware of frequent payer audits targeting incorrect use of high-level CPT® codes like 99215 or 90837.
Quick Toolkit for Clinicians and Billing Teams
- Top 25 CPT® Codes Chart – Laminated or PDF reference.
- Modifier Reference Guide – Explains common modifiers.
- Lookup Decision Tree – AMA vs. EHR vs. subscription tool.
- ICD-10 to CPT® Crosswalk – For fast pairing of diagnoses and procedures.
Conclusion
Looking up and using the right CPT® code isn’t just a back-office task—it’s a critical part of clinical care and financial sustainability. Whether you’re a solo practitioner, part of a hospital team, or a billing specialist, having a system to identify, apply, and verify CPT® codes can save time, reduce denials, and boost reimbursement. With the proper tools, consistent updates, and awareness of guidelines, coding becomes a seamless extension of your documentation process.
Experience seamless, AI-powered documentation with DocScrib.
Streamline your clinical workflow and reduce admin burden.
Click here to book your free demo.