Updated on: July 20, 2025
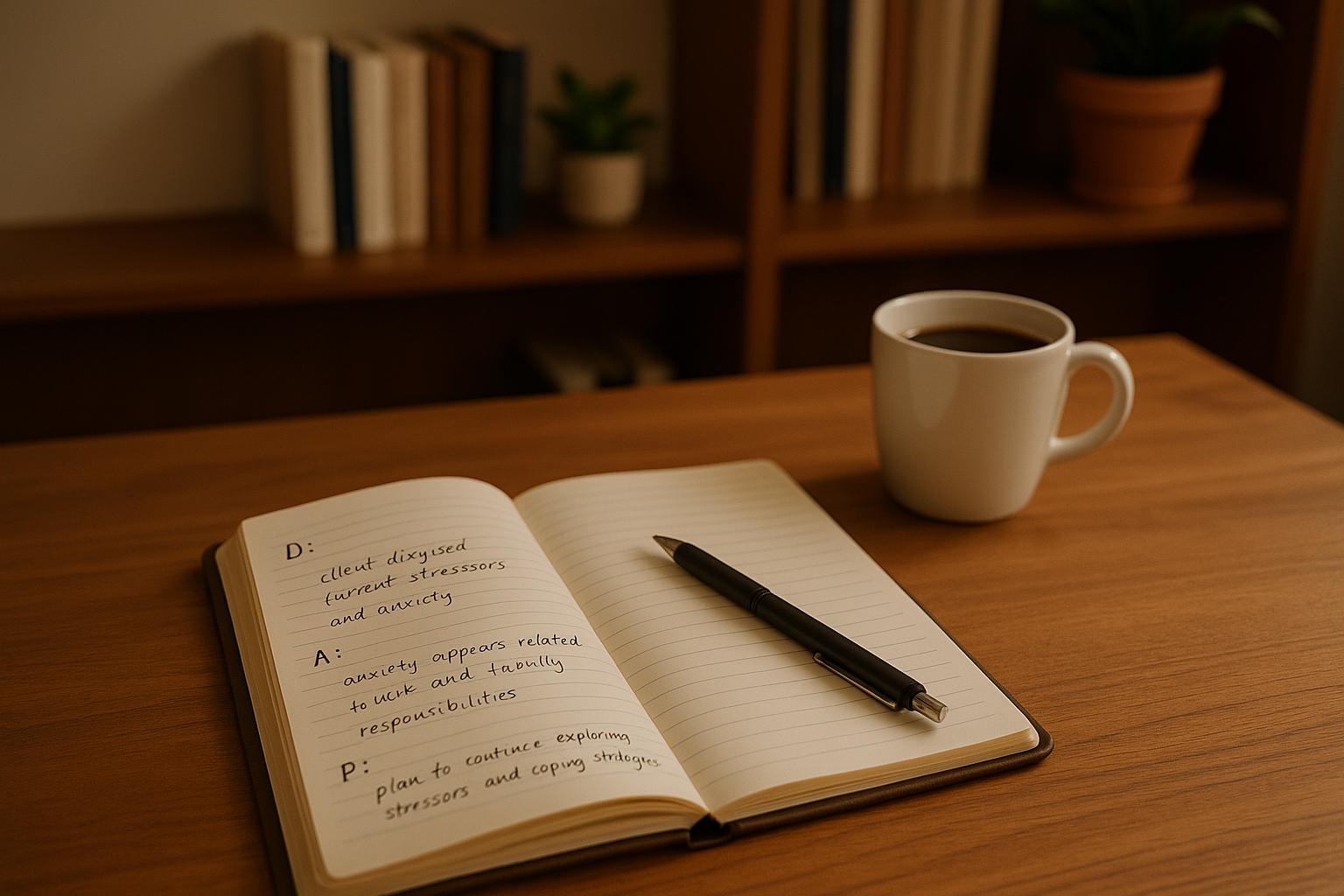
DAP notes are a structured way for therapists to document sessions, combining client-reported symptoms, observations, and treatment plans into three sections: Data, Assessment, and Plan. This format helps therapists save time, ensure compliance with legal and insurance standards, and improve treatment tracking. Here’s a quick breakdown:
- Data: Record objective details like client-reported symptoms, mood, and behavior during the session. Example: "Client reported trouble sleeping and appeared tense."
- Assessment: Analyze the data, highlight progress or challenges, and make clinical impressions. Example: "Client’s anxiety level increased to 7/10 due to work stress."
- Plan: Outline next steps, interventions, or assignments. Example: "Practice mindfulness exercises; follow up next session."
Using templates and tools like AI-driven platforms can make writing DAP notes faster and more accurate, freeing up time for patient care. Prioritize clarity, brevity, and actionable steps in your notes.
How to Write DAP Notes in Private Practice: A Therapist’s Guide
Understanding the DAP Format: Components and Best Practices
The DAP format organizes therapy documentation into three clear sections: Data, Assessment, and Plan. Each section plays a distinct role in creating structured and effective clinical records.
Data: Recording Patient Information and Observations
The Data section is all about recording factual, objective information gathered during the session. This includes what you observe and what your client reports – no interpretations, just the facts.
"In the data section, you will include information you observed in the session. In this section, mental health professionals should record any data about the client, including client reports of symptoms and mental status." – Marissa Moore, LPC, LCPC
Here’s what to include in this section:
- The client’s appearance and any noticeable changes.
- Direct quotes that highlight key concerns or insights.
- Details about the client’s presenting problem.
- Observations of mood, affect, thought processes, and behavior.
- Results from any assessments or screening tools used during the session.
For example, if a client shares specific worries or you notice changes in their demeanor, document these details. Direct quotes are especially useful when they capture the client’s thoughts or concerns in their own words.
Assessment: Writing Clinical Impressions
In the Assessment section, you analyze the data and draw clinical conclusions. This is where you interpret the information, identify patterns, and make connections. Include your clinical impressions and any diagnoses, referencing diagnostic criteria like DSM-5 codes when applicable.
Use this section to:
- Assess the client’s progress toward treatment goals.
- Highlight new challenges or areas of improvement.
- Conduct a risk assessment if there’s potential harm to self or others.
For instance, imagine a client with Generalized Anxiety Disorder who reports increased work-related stress. They might describe symptoms such as muscle tension and trouble concentrating while also showing improvement in recognizing anxiety triggers. However, challenges like anticipatory anxiety might still affect their daily life. By linking these observations to clinical impressions, you create a clear narrative that supports your conclusions.
This step ensures that your analysis directly informs the treatment plan, making it both logical and actionable.
Plan: Documenting Next Steps and Interventions
The Plan section outlines what comes next. Based on your clinical impressions, this is where you detail interventions and strategies to address the client’s needs. Be specific about the steps to be taken.
Include:
- Interventions tied to each identified issue.
- Homework assignments or tasks for the client to complete between sessions.
- Referrals or collaboration with other providers, if needed.
- Follow-up plans to track progress.
For example, if the client struggles with anxiety, you might recommend mindfulness exercises or schedule a follow-up to review their coping strategies. By connecting interventions to treatment goals, this section creates a roadmap for ongoing care and progress monitoring.
This structured approach ensures continuity and keeps both the therapist and client focused on clear, measurable outcomes.
How to Write DAP Notes More Efficiently
Writing DAP notes doesn’t have to eat into your personal time. With the right approach, you can create clear, compliant documentation while maintaining a healthy work-life balance and delivering the quality care your clients expect.
Using Templates to Simplify Your Workflow
Templates can take the stress out of starting from scratch every time you write a DAP note. They provide a structured format that ensures your documentation is consistent and complete.
Good templates include pre-formatted sections with labeled fields like "Client’s response" or "Session goals", making it easy to input key information. Some templates even feature drop-down menus and checklists for common observations and interventions, while still leaving room for personalized details.
To make your templates even more effective, add specific prompts for each DAP section. For example:
- Data Section: Include fields for mood observations, direct quotes, and notable behavioral changes.
- Assessment Section: Use checkboxes for progress markers and risk factors.
- Plan Section: Provide standardized intervention categories with space for tailoring specific strategies.
Standardizing templates across your practice ensures consistency and makes collaboration easier for your team. Training everyone on the DAP format can further streamline transitions and improve communication.
Don’t forget to review and update your templates regularly. As guidelines, laws, or your clinical preferences evolve, your templates should reflect those changes. What works now might need tweaking as your methods or client base shift.
Once your templates are in place, the next step is mastering the art of writing concise yet detailed notes.
Striking the Right Balance Between Detail and Brevity
Templates are a great start, but efficient DAP notes also require a balance between providing enough detail and keeping it brief. Aim for 150-300 words that capture the essential points without overloading your documentation.
Adjust word counts based on session type. For example, standard outpatient therapy sessions (45–60 minutes) typically need 175–275 words, while shorter medication management visits (20 minutes) might only require 120–180 words. High-acuity sessions, like those involving crisis management, may justify up to 350 words.
Focus on documenting information that supports the client’s diagnosis, explains your treatment decisions, and outlines your therapeutic approach. Every sentence should have a purpose, whether it’s noting observable changes, justifying clinical decisions, or guiding future care.
- In the Data section, use bullet points or brief quotes instead of lengthy narratives. Include direct quotes only when they provide significant insights, and avoid transcribing entire conversations.
- For the Assessment section, tie your impressions to measurable outcomes, like rating scales or SMART goals. Instead of vague notes like "client seemed anxious", write something more specific, such as "client reported an anxiety level of 7/10, up from 4/10 last session."
- Timing is crucial. Documentation completed more than 24 hours after a session often loses 40% of its detail accuracy. Writing notes immediately after a session helps ensure accuracy and completeness.
Trim any unnecessary quotes or details, and move non-essential information to collateral notes. Be sure to include follow-up dates or note if they’re not applicable. This approach keeps your DAP notes focused and relevant while ensuring they remain comprehensive and clinically useful.
sbb-itb-5a50404
Common DAP Note Mistakes and How to Fix Them
Even seasoned therapists can sometimes slip into documentation habits that weaken their DAP notes. By sticking to the structured DAP format and steering clear of common pitfalls, you can improve clarity and create more effective treatment plans. Strengthening your documentation not only enhances your practice but also better addresses your clients’ needs.
Writing Specific Instead of Vague Observations
A common issue in DAP notes is the use of vague or generalized language that lacks essential detail. For example, simply stating a client "seemed anxious" doesn’t provide enough information. Instead, focus on what you can observe directly – behaviors, measurable data, and actions that give a fuller picture of the session.
"When you document client behaviors during therapy sessions, use specific, objective terms that convey your observations accurately."
- Vivian Chung Easton, LMFT, CHC, Clinical Product Lead @ Blueprint
Replace unclear descriptions like "seemed anxious" with specific observations such as "fidgeting, rapid speech, and shallow breathing." This approach not only clarifies the client’s emotional state but also ties your observations to treatment goals. Avoid subjective terms like "seems", "appears", or "maybe" in the Data section, as they can make your documentation less precise. Stick to what you can see and measure.
Creating Clear Follow-Up Plans
While detailed observations shape your clinical impressions, a clear and actionable follow-up plan ensures these insights lead to progress. The Plan section should detail the next steps for advancing treatment. This might include scheduling the next session, recommending specific therapeutic interventions, or revising treatment goals based on what occurred during the session. Every plan should answer the critical question: "What happens next?"
Using SMART goals – specific, measurable, achievable, relevant, and time-bound – can help ensure your plans are realistic and trackable. For example, you might assign homework with a clear deadline or outline measurable objectives for future sessions.
Be thorough when documenting referrals, scheduling, or next session details. If you’re referring a client to another provider or service, include all relevant information, like contact details and deadlines.
For clients with safety concerns, integrate crisis planning into your notes by referencing established safety protocols and detailing steps to take if symptoms worsen. For instance, a well-crafted plan for a client managing depression might include scheduling the next session, assigning a thought record chart to track automatic negative thoughts, providing referrals to financial advisors, and ensuring the client follows a pre-established safety plan if their condition deteriorates.
Using DocScrib for DAP Notes

AI-powered tools are reshaping how clinicians handle documentation, and DocScrib is at the forefront of this shift. On average, clinicians dedicate about 13.5 hours each week to documentation – a figure that has risen by 25% since 2015. Even more striking, 44% of that time involves repetitive tasks. DocScrib’s AI-driven platform simplifies the process of writing DAP notes, potentially reducing documentation time by up to 70%. This means therapists can spend more time doing what truly matters – caring for their patients.
Customizable DAP Templates
DocScrib offers templates that automatically structure notes into the Data, Assessment, and Plan sections, with flexible fields to align with your practice’s needs. The platform’s AI continuously adapts to your unique documentation habits, learning your preferred terms and style to ensure your notes consistently reflect your clinical voice. This customization also extends to real-time documentation, making the process even more seamless.
Real-Time Transcription and Note Automation
With its real-time transcription tools, DocScrib transforms spoken therapy sessions into structured clinical notes automatically. By leveraging natural language processing and machine learning, the platform converts unstructured audio into accurate and well-organized DAP notes.
The AI categorizes session content into the DAP framework, saving clinicians up to an hour each day. As it learns your writing preferences, the system becomes increasingly tailored to your style, cutting down on the need for extensive post-session edits.
HIPAA-Compliant Storage and EHR Integration
DocScrib prioritizes security with HIPAA-compliant measures like encryption, two-factor authentication, and role-based access. It also integrates directly with electronic health record (EHR) systems, eliminating duplicate work. Whether your EHR supports basic copy-paste functionality or full API integration, DocScrib fits seamlessly into your workflow. Clinics using AI alongside their EHR systems report saving 2–4 hours daily, time that can be redirected to patient care.
Additionally, DocScrib includes regular security audits and detailed access controls, allowing administrators to manage who can view, edit, or export documentation. These features not only ensure compliance but also give clinicians the freedom to focus more on their patients.
Conclusion: Improving DAP Notes for Better Patient Care
Mastering DAP notes – Data, Assessment, and Plan – is a powerful way to streamline documentation and enhance clinical outcomes. This structured approach ensures that essential session details are captured clearly and effectively, keeping the focus on actionable steps. By documenting specific observations, connecting them to evidence-based assessments, and outlining follow-up plans, therapists can deliver higher-quality care.
Good documentation isn’t just about keeping records – it’s a cornerstone of effective treatment and legal protection. Thoughtful and well-organized DAP notes help maintain continuity of care, improve treatment tracking, and safeguard both therapists and clients. Therapists who refine their note-taking skills often notice improvements in their clinical decisions, as clear documentation fosters better analysis and planning.
Time-efficient documentation also has a direct impact on patient care. Reducing the time spent on paperwork allows therapists to focus more on building therapeutic relationships and planning effective treatments. Studies show that U.S. therapists dedicate 11–15 hours a week to documentation, but with efficient tools, that time can drop by as much as 30%. These time savings open the door to integrating advanced tools into practice.
AI-powered tools like DocScrib take documentation efficiency to the next level. By automating repetitive tasks and offering structured DAP templates, these platforms help therapists maintain high standards without sacrificing time with clients. Features like real-time transcription, customizable templates, and HIPAA-compliant storage ensure that documentation becomes a support system rather than a burden, enabling therapists to focus on what truly matters – patient care.
FAQs
How can AI tools like DocScrib help therapists write better DAP notes more efficiently?
AI tools such as DocScrib simplify the process of writing DAP notes by automating repetitive tasks, reducing errors, and ensuring adherence to clinical documentation standards. This frees up therapists’ time, enabling them to dedicate more attention to their clients rather than getting bogged down with paperwork.
DocScrib offers smart suggestions and structured templates specifically designed for the DAP format, making it easier for therapists to produce clear, concise, and professional notes. By cutting down on the effort required for manual documentation, AI-driven platforms not only save time but also improve the overall quality and accuracy of therapeutic records.
What are common mistakes therapists make when writing DAP notes, and how can they prevent them?
Therapists sometimes slip into common pitfalls like writing notes that are too vague, adding irrelevant details, letting personal biases seep in, or straying from the treatment goals. These mistakes can result in documentation that’s unclear or not particularly useful.
To keep your notes effective, aim for them to be specific, concise, and objective. Center your writing on the client’s progress and how it aligns with their treatment plan. Stick to the key points – there’s no need for overexplaining or adding personal opinions. Clear and well-structured notes not only make documentation more useful but also support better outcomes in therapy.
Why is it essential to use clear and specific observations in the Data section of DAP notes?
Using clear and precise observations in the Data section is key to keeping your documentation accurate, objective, and straightforward. Including specific details helps create a reliable basis for evaluating a client’s progress and developing effective treatment plans.
On the other hand, vague or overly broad descriptions can cause misunderstandings, misinterpretations, or missed chances to tackle important therapy concerns. By zeroing in on observable facts – like the client’s words, actions, or emotional reactions – you ensure your notes remain professional and practical.